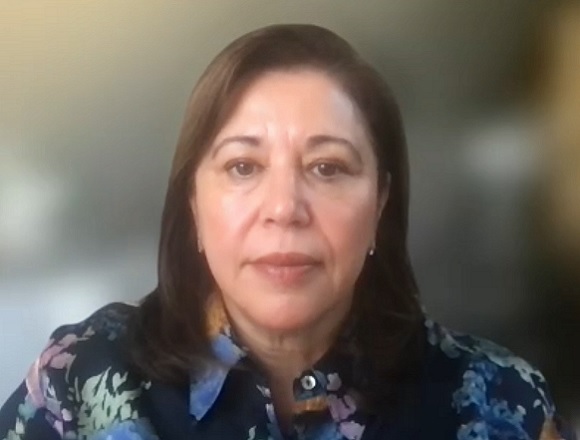
Alexandra Papaioannou, MD, MSc, is a professor of medicine in the Divisions of Geriatric Medicine & Rheumatology at McMaster University and the lead investigator for the Long-term Care Ontario Osteoporosis Strategy. She has expertise in clinical practices that involve osteoporosis and frailty in older adults.
Can a patient treated with bisphosphonates or denosumab undergo invasive dental procedures? How to manage such a patient?
Alexandra Papaioannou, MD, MSc: Yes, they can definitely go through invasive dental procedures. Bisphosphonates should be stopped at least a week prior to the treatment. The dental instruction is to wait a month, 4 weeks, before the bone heals. With denosumab, have [the procedure] towards the end of the 6 months after the injection, and you can wait one month—delay the injection up to a month after.
In the meantime, in individuals who are at risk ensure that they are doing dental care 3 times a day even before starting these drugs. See their dentist to assess, do they have periodontal disease? Are they smokers? On alcohol? Have them modify those risk factors. If they’re on immunosuppressive drugs like steroids, those individuals are at higher risk and should be monitored more frequently. So, it’s important to check what other drugs your patient is receiving. Certainly, those who are on higher doses of these drugs for underlying malignancy are at a much higher risk.
 English
English
 Español
Español
 українська
українська