Transfusion strategies in nonbleeding critically ill adults: European guidelines in a nutshell. Part 1
The guidelines from the European Society of Intensive Care Medicine (ESICM) provide recommendations and suggestions (conditional or weak recommendations) on the transfusion of different blood products, including platelets and plasma, in nonbleeding critically ill adults.
Strong recommendations are issued when most individuals would want the recommended course of action. Clinicians should adhere to this course of action in most situations and would need a compelling reason not to follow it. These recommendations may also provide a framework for hospital-based transfusion policies and benchmarks for performance measures. With weak recommendations (suggestions), the majority of patients would want the suggested course of action but many would not, and clinicians should tailor their actions to individual circumstances and to patient values and preferences. This recommendation scheme is part of the widely used GRADE system.
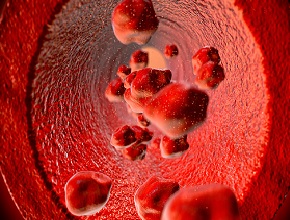
The ESICM guideline authors state that although benefits of blood product transfusion may be intuitive, they are also associated with risks, including hemolysis, acute lung injury, and volume overload.
In terms of red blood cell transfusions, the recommendations are:
- In favor of a restrictive transfusion threshold (70 g/L) versus a liberal transfusion threshold (90 g/L) in most populations, including those with acute respiratory distress syndrome (ARDS) (moderate quality of evidence/certainty/confidence; see exclusions below).
- In favor of a restrictive transfusion threshold (75 g/L) versus a liberal transfusion threshold (85-90 g/L) in adults undergoing cardiac surgery (moderate confidence).
In terms of red blood cell transfusions, the suggestions (weak recommendations) are:
- In favor of a liberal transfusion threshold (90-100 g/L) versus a restrictive threshold (70 g/L) in patients with acute coronary syndromes (low confidence).
- In favor of a restrictive transfusion threshold (70 g/L) versus a liberal transfusion threshold (90 g/L) in patients with sepsis and septic shock (moderate confidence).
- In favor of a restrictive transfusion threshold (70 g/L) versus a liberal transfusion threshold (90 g/L) in patients with prolonged weaning from mechanical ventilation (low confidence).
- In favor of using hemoglobin concentration or hematocrit to guide transfusion thresholds versus using acidosis, arrhythmia, electrocardiographic (ECG) changes, or mixed or central venous blood oxygenation for this purpose.
The authors also identified populations of anemic patients in whom they could not make recommendations and stated that both liberal and restrictive strategies remain appropriate pending further data:
- Patients with acute neurologic injury (eg, traumatic brain injury, subarachnoid hemorrhage, stroke).
- Patients undergoing venovenous or venoarterial extracorporeal membrane oxygenation (ECMO).
- Patients with oncologic and hematologic-oncologic conditions.
- Elderly patients: The panel recognized that with advancing age the potential benefits and harms of transfusion might differ. There was insufficient evidence to suggest a clear age threshold where the other transfusion guidelines would no longer apply; indeed, many of the randomized trials evaluated for the guideline had “elderly” populations (mean age, ~65 years). However, whether this evidence still applies to those who are >80 or >90 years of age is unclear.
What platelet counts are acceptable when performing thoracentesis or lumbar puncture? Click here to submit your answers via MetaClinician and see what your peers would do.
 English
English
 Español
Español
 українська
українська