Thrombotic thrombocytopenia following administration of the ChAdOx1 nCov-19 vaccine
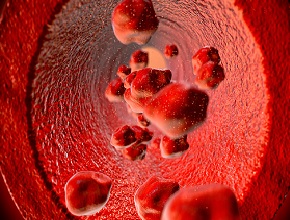
Background: In recent weeks there have been reports of venous thrombosis occurring at unusual sites in association with thrombocytopenia, which have developed after vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with the ChAdOx1 nCov-19 (AstraZeneca) vaccine.
Methods: In this study 28 patients were assessed for suspected vaccine-associated thrombotic events, among whom detailed clinical and laboratory features were available for 11 patients. A standard enzyme-linked immunosorbent assay (ELISA) was used to detect platelet factor 4 (PF4)–heparin antibodies, and a modified (PF4-enhanced) platelet-activation test was used to detect platelet-activating antibodies under various reaction conditions. This testing was done on blood samples from patients who were referred for investigation of vaccine-associated thrombotic events, with 28 testing positive on a screening PF4–heparin immunoassay.
Results: Of the 11 patients with available clinical and laboratory details (9 women; median age, 36 years; range, 22-49 years), 10 presented with ≥1 thrombotic events 5 to 16 days after vaccination and 1 presented with fatal intracranial bleeding. In the 10 patients with thrombotic events, 9 had cerebral venous thrombosis, 3 had splanchnic vein thrombosis, 3 had pulmonary embolism, and 4 had other thromboses; of these patients, 6 died. There were 5 patients with disseminated intravascular coagulation. None of these patients had received heparin before the onset of symptoms.
Conclusions: These findings indicate that receipt of the AstraZeneca SARS-CoV-2 vaccine can lead to the development of immune thrombotic thrombocytopenia mediated by platelet-activating antibodies against PF4, which mimics autoimmune heparin-induced thrombocytopenia (HIT). This entity is now referred to as vaccine-induced immune thrombotic thrombocytopenia (VITT).
McMaster editors' comment: Autoimmune or spontaneous HIT occurring in the absence of antecedent heparin exposure is a very rare disease, which appears to be triggered by an unknown antigen that is part of the AstraZeneca vaccine. This syndrome has recently been described to occur in association with another adenovirus vector vaccine against SARS-CoV-2, manufactured by Johnson & Johnson. The treatment of VITT is anchored on high-dose (1 g/kg) intravenous immunoglobulin. As with HIT, nonheparin anticoagulants are administered—such as fondaparinux, argatroban, or a direct oral anticoagulant—and platelet transfusions are avoided. The high mortality associated with early cases of undiagnosed VITT likely reflects the well-intentioned but inappropriate use of heparin, which can worsen the prothrombotic diathesis. VITT is a potentially serious but extremely rare adverse event, occurring in 1 per 100,000 recipients of the AstraZeneca vaccine (European Medicines Agency, April 23, 2021). The benefits of vaccination, which include preventing coronavirus disease 2019 (COVID-19) alongside hospitalizations and thrombotic events related to COVID-19, far outweigh the risk of VITT.
 English
English
 Español
Español
 українська
українська