Li L, Yang G, Zhao L, et al. Baseline Demographic and Clinical Characteristics of Patients with Adrenal Incidentaloma from a Single Center in China: A Survey. Int J Endocrinol. 2017;2017:3093290. doi: 10.1155/2017/3093290. Epub 2017 Aug 7. PMID: 28848603; PMCID: PMC5564109.
Lee JM, Kim MK, Ko SH, et al; Korean Endocrine Society, Committee for Clinical Practice Guidelines. Clinical Guidelines for the Management of Adrenal Incidentaloma. Endocrinol Metab (Seoul). 2017 Jun;32(2):200-218. doi: 10.3803/EnM.2017.32.2.200. PMID: 28685511; PMCID: PMC5503865.
Fassnacht M, Arlt W, Bancos I, et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2016 Aug;175(2):G1-G34. doi: 10.1530/EJE-16-0467. PMID: 27390021.
Kapoor A, Morris T, Rebello R. Guidelines for the management of the incidentally discovered adrenal mass. Can Urol Assoc J. 2011 Aug;5(4):241-7. doi: 10.5489/cuaj.11135. Erratum in: Can Urol Assoc J. 2012 Aug;6(4):244. PMID: 21801680; PMCID: PMC3147036.
Zeiger MA, Thompson GB, Duh QY, et al; American Association of Clinical Endocrinologists; American Association of Endocrine Surgeons. American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons Medical Guidelines for the Management of Adrenal Incidentalomas: executive summary of recommendations. Endocr Pract. 2009 Jul-Aug;15(5):450-3. doi: 10.4158/EP.15.5.450. PMID: 19632968.
Barzon L, Sonino N, Fallo F, Palu G, Boscaro M. Prevalence and natural history of adrenal incidentalomas. Eur J Endocrinol. 2003 Oct;149(4):273-85. doi: 10.1530/eje.0.1490273. PMID: 14514341.
Definition, Etiology, PathogenesisTop
Incidentally found adrenal lesions >1 cm are detected on imaging (computed tomography [CT] or magnetic resonance imaging [MRI]) in up to 4% of the general population undergoing CT imaging for a variety of reasons and up to 10% of patients aged >70 years. They can be functioning or nonfunctioning and benign or malignant. In most cases they are nonfunctioning, benign adrenocortical adenomas.
Most adrenal lesions are unilateral but up to 15% are bilateral. The peak incidence is in the sixth and seventh decades of life, with a mean age of 55 years. Adrenal incidentalomas are more common in women.
Possible etiologies of adrenal incidentalomas:
1) Adrenal adenomas (80% of cases):
a) Nonfunctioning (most common).
b) Functioning: From most common to rare: Cushing syndrome, primary aldosteronism, and feminizing or masculinizing tumors.
2) Pheochromocytoma (5%).
3) Primary adrenocortical carcinoma (ACC) (6%-12%): Most are functioning (Cushing syndrome; 60%) and usually large (>6 cm).
4) Metastatic (2%-3%): From most common to less frequent: originating in the lung, gastrointestinal (GI) tract, kidney, breast; melanoma; lymphoma. These are usually <4 cm and often bilateral.
5) Other (<8%): Cysts, hemangioma, infection (tuberculosis, fungi), granulomatous disease (sarcoidosis), myelolipoma, ganglioneuroma, neuroblastoma, primary bilateral macronodular hyperplasia.
Clinical Features and Natural HistoryTop
Most patients are asymptomatic and tend to have a normal biochemical profile. However, they need to undergo a careful clinical and biochemical evaluation for adrenal hormone excess (pheochromocytoma, primary aldosteronism, Cushing syndrome, feminization/virilism) and the risk of malignancy.
Most adrenal masses are benign (>90%) and nonfunctioning and remain biochemically and radiographically stable. Some masses increase in size and secrete hormones over time.
The following characteristics are suspicious for malignancy (a suspicious adrenal incidentaloma) and require further evaluation and follow-up:
1) History: Primary malignancy (lung, breast, kidney, GI tract, melanoma).
2) Radiologic features:
a) Heterogenous; irregular margins and shape.
b) Attenuation ≥10 Hounsfield units (HU) and contrast avidity (a low relative and absolute washout percentage).
c) Location/distribution: Bilateral; lymph node involvement.
d) Size: ≥4 to 6 cm (25% of lesions >4 cm are ACC cases).
e) Growth: >0.5 to 1 cm over 3 to 6 months.
DiagnosisTop
The most important questions to consider are whether the incidentaloma is malignant or benign and whether it is functioning or nonfunctioning.
Although most adrenal incidentalomas are benign and nonfunctioning, biochemical testing for pheochromocytoma, Cushing syndrome, primary aldosteronism, sex hormone–producing tumors, and adrenal insufficiency should be performed as indicated clinically and by imaging characteristics. Rarely fine-needle aspiration biopsy (FNAB) may be needed.
1. Biochemical tests: The following should be performed as indicated:
1) If the patient has hypertension, perform aldosterone and renin evaluations to calculate the aldosterone-to-renin ratio (ARR) and screen for primary aldosteronism. ARR interpretation depends on age, drug interference, menstrual cycle, and other comorbidities. Also see Primary Aldosteronism.
2) To exclude pheochromocytoma, evaluate 24-hour urine fractionated metanephrine levels or plasma metanephrine levels. Also see Pheochromocytoma and Paraganglioma.
3) To exclude Cushing syndrome, perform the 1-mg oral dexamethasone suppression test at 23:00 followed by measurement of serum cortisol levels at 8:00 the next morning. Cortisol levels ≤50 nmol/L exclude Cushing syndrome. Also see Cushing Syndrome.
4) In case of ACC suspicion or clinical features of feminization or masculinization, also evaluate serum testosterone, dehydroepiandrosterone sulfate (DHEAS), and estradiol.
5) If there is clinical suspicion of adrenal insufficiency or bilateral lesions, evaluate morning cortisol and adrenocorticotropic hormone (ACTH) with or without cosyntropin (INN tetracosactide) stimulation to exclude adrenal insufficiency. Also see Primary Adrenal Insufficiency (Addison Disease).
2. Imaging studies: On CT scanning, features suggestive of a benign adrenal mass are size <4 cm, homogenous morphology, smooth contour, round border, annual growth <1 cm, low tumor density (attenuation <10 HU; this has 98% sensitivity and 71% specificity for benign adrenal masses), and >40% relative and >60% absolute washout with contrast. MRI may add extra information in selected cases.
3. FNAB is performed rarely, in patients with lesion(s) suspected to arise from extra-adrenal metastasis or infection. Biopsy can provide information about the type and stage of primary cancer, but it does not reliably differentiate between a benign and a malignant primary adrenal lesion. Biopsy should not be performed if pheochromocytoma is suspected due to the risk of a catecholamine crisis.
TreatmentTop
Clinicians should have a parallel approach in managing adrenal incidentalomas for assessing the malignant potential and possible functional hormonal status of the lesion (Figure 6.1-1).
Consider surgical resection referral in patients with a tumor size >4 to 6 cm, growth rate >20% and >0.5 cm in the maximum diameter over 3 to 6 months, characteristic radiologic features of a nonbenign tumor, hyperfunctioning tumor, or isolated metastatic lesion from non–small cell lung cancer.
Follow-UpTop
The following applies to patients receiving follow-up care and to those undergoing surveillance of nonresected lesions.
1. Clinical evaluation for signs and symptoms of hormone excess should be performed every 6 to 12 months for 5 years after the initial diagnosis.
2. Biochemical evaluation should be performed at baseline for hormone excess and later as clinically indicated or in case of increase in size of the incidentaloma.
3. Imaging studies in most cases should be repeated once at 6 to 12 months, or earlier at 3 months if there are any suspicious features. The CT scan should be carefully reviewed for size, attenuation/HU, and contrast washout. CT imaging should be repeated subsequently in patients with a 15% increase in incidentaloma size but still a low risk of carcinoma. No imaging follow-up is usually required in those with lesions ≤2 cm and ≤10 HU.
Patients with a normal biochemical evaluation and stable or low-risk radiographic imaging results may be considered for discontinuation of follow-up after 5 years from the initial diagnosis.
FiguresTop
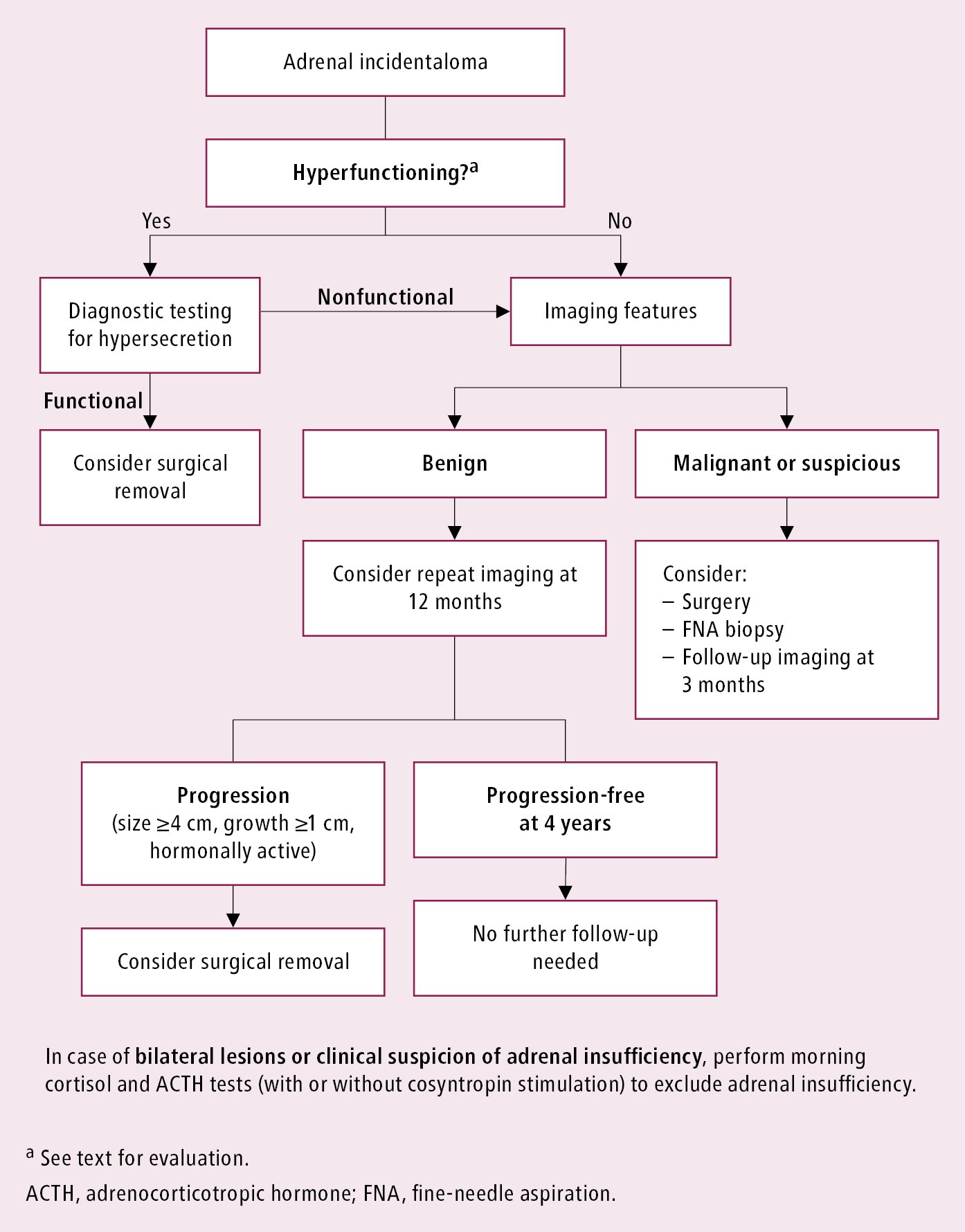
Figure 6.1-1. Approach to adrenal incidentalomas.