Hew-Butler T, Rosner MH, Fowkes-Godek S, et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, California, 2015. Clin J Sport Med. 2015 Jul;25(4):303-20. doi: 10.1097/JSM.0000000000000221. PMID: 26102445.
Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. doi: 10.1530/EJE-13-1020. Print 2014 Mar. Erratum in: Eur J Endocrinol. 2014 Jul;171(1):X1. PMID: 24569125.
Verbalis JG, Goldsmith SR, Greenberg A, et al. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med. 2013 Oct;126(10 Suppl 1):S1-42. doi: 10.1016/j.amjmed.2013.07.006. PMID: 24074529.
Definition, Etiology, PathogenesisTop
Hyponatremia is defined as a serum [Na+] <135 mmol/L.
In the majority of cases, hyponatremia is a consequence of water disturbances that result in a relative excess of body water compared with the body sodium content. The most frequent cause is impaired renal free water excretion due to inappropriate arginine vasopressin (AVP) (previously known as antidiuretic hormone [ADH]) hypersecretion caused by nonosmotic factors. Less frequently, the relative excess of body water may be due to excessive free water intake, which exceeds renal capacity for free water excretion.
Severity of hyponatremia:
1) Mild ([Na+], 130-134 mmol/L).
2) Moderate ([Na+], 125-129 mmol/L).
3) Severe ([Na+] <125 mmol/L).
Classification of hyponatremia based on its duration:
1) Acute hyponatremia is that of a documented duration <48 hours.
2) Chronic hyponatremia is that of a documented duration ≥48 hours, or any case of hyponatremia of undocumented duration unless clinical features and history indicate acute hyponatremia.
Classification of hyponatremia based on plasma osmolality (measured, not calculated!), and volume status:
1) Hypotonic hyponatremia: Sodium ions are the key extracellular osmolyte. Low serum [Na+] is most commonly associated with a hypotonic extracellular fluid (ECF) and a shift of water from the ECF to the intracellular fluid (ICF), which leads to cellular swelling. The most frequent cause of hypotonic hyponatremia is water retention due to syndrome of inappropriate antidiuresis (SIAD) (previously syndrome of inappropriate antidiuretic hormone secretion [SIADH]).
a) Hypotonic hyponatremia with hypovolemia is caused by sodium and water loss that is partially replaced with fluids containing no electrolytes. Water and sodium may be lost via the skin (excessive sweating), gastrointestinal (GI) tract (vomiting, diarrhea, GI fistulas), kidneys (mainly loss of sodium due to diuretic use; mineralocorticoid deficiency; osmotic diuresis caused by hyperglycemia, urea, or mannitol; salt-losing nephritis; or congenital or acquired tubulopathy), or a shift of fluids into the “third space.”
b) Hypotonic hyponatremia with euvolemia, the most frequent type of hyponatremia, is caused by SIAD (see above), glucocorticoid deficiency, use of thiazide diuretics, prolonged strenuous exercise, primary polydipsia, long-term use of a low-sodium diet, hypothyroidism, increased sensitivity to AVP, or mutations of genes encoding V2 or aquaporin 2 receptors.
c) Hypotonic hyponatremia with hypervolemia is caused by increased AVP secretion in patients with a relative decrease in effective intravascular volume (chronic heart failure [HF], cirrhosis with ascites, nephrotic syndrome with edema) or by excessive intake of fluids containing no electrolytes in patients with impaired free water excretion (acute kidney injury, advanced chronic kidney disease).
2) Nonhypotonic (isotonic or hypertonic) hyponatremia, also called translocational hyponatremia, is caused by an increase in plasma concentrations of effective osmolytes leading to a shift of water from the ICF to the ECF and subsequent hyponatremia due to dilution. Depending on plasma concentrations of osmolytes, plasma osmolality may be normal or increased. The most frequent cause is severe hyperglycemia (when correcting sodium in the presence of hyperglycemia, add ~3.5 mmol/L to the sodium concentration for every 10 mmol/L increment in the glucose level >10 mmol/L). Less frequent causes include IV infusions of mannitol; administration of high doses of hyperosmolal contrast media; or leakage of isotonic mannitol, sorbitol, or glycine to blood during transurethral prostate resection.
Pseudohyponatremia is a falsely low serum [Na+] caused by high plasma lipid or paraprotein levels. Plasma osmolality is normal.
Clinical FeaturesTop
Clinical manifestations depend on the severity and rate of plasma sodium level decrease, effective plasma osmolality, and direction and magnitude of blood volume changes.
In the majority of patients with slowly developing mild to moderate hyponatremia, no serious central nervous system (CNS) symptoms are seen, but impaired concentration, impaired cognitive functions, and dizziness may occur. Neurologic manifestations of hyponatremia depend on the severity and rate of plasma sodium level decrease and the resulting changes in plasma osmolality. They may be:
1) Moderate, including nausea (without vomiting), confusion, and headache.
2) Severe, including vomiting, somnolence, seizures, and coma (Glasgow coma score ≤8).
Note: These manifestations are nonspecific and may have other causes.
Acute hyponatremia is suspected in the following clinical situations (in patients with undocumented duration of hyponatremia): postoperative period, polydipsia, after or during strenuous exercise, recently started treatment with thiazide diuretics, preparation to colonoscopy, treatment with IV cyclophosphamide, amphetamine use, recently started treatment with AVP analogues.
Clinical features suggestive of dehydration and hypovolemia include dry mucous membranes, reduced skin turgor, orthostatic or constant hypotension, tachycardia, and decreased urine output.
DiagnosisTop
Diagnostic algorithm in hyponatremia: Figure 5.2-1.
Hyponatremia is diagnosed in patients with serum [Na+] <135 mmol/L after pseudohyponatremia has been excluded (see below).
1. At the beginning of workup, exclude hyperglycemia and measure plasma osmolality to establish whether the patient has hypotonic or nonhypotonic (isotonic or hypertonic) hyponatremia. Nonhypotonic hyponatremia may be due to only a few known causes (most frequently severe hyperglycemia) and is not associated with a risk of neurologic complications (cerebral edema, osmotic demyelination syndrome [ODS]).
2. In patients with isotonic hyponatremia, exclude pseudohyponatremia. Determination of [Na+] in a nondiluted serum sample using ion-selective electrodes provides accurate values. If this technique is not available, measure serum triglyceride, cholesterol, and total protein levels.
3. In patients with hypotonic hyponatremia, measure urine osmolality (Uosm) and urine sodium level (UNa) in the same urine sample or in separate urine samples collected at the same time.
In patients with Uosm ≤100 mmol/kg H2O, hyponatremia is caused by a relative excess of water resulting from polydipsia, long-term use of a low-solute diet (eg, in patients with anorexia or those following a diet based on biscuits and tea or beer), or excessive intake of fluids containing no electrolytes (particularly in patients with impaired kidney function).
In patients with Uosm>100 mmol/kg H2O, measure UNa:
1) In patients with UNa ≤30 mmol/L, hyponatremia may be caused by low effective intravascular volume. Estimate water content in the ECF based on clinical data.
a) In patients with increased ECF water content (edema, effusions to body cavities), hyponatremia may be caused by HF, cirrhosis, or nephrotic syndrome.
b) In patients with decreased ECF water content (features of dehydration and hypovolemia), hyponatremia may be caused by loss of water and sodium via the GI tract, skin, or due to a shift of water to the “third space”; or by diuretic treatment (with information about treatment either lacking or concealed by the patient).
2) Patients with UNa>30 mmol/L should be assessed for kidney disease or diuretic treatment (or both).
a) In patients who have no kidney disease and do not use diuretics, estimate ECF water content on the basis of clinical data. In patients with normal ECF water content, hyponatremia is most frequently caused by SIAD. Other possible causes include glucocorticoid deficiency (secondary adrenal insufficiency), diuretic treatment (with information about treatment either lacking or concealed by the patient), and severe hypothyroidism. In patients with decreased ECF water content, hyponatremia may be caused by vomiting, mineralocorticoid deficiency (primary adrenal insufficiency), diuretic treatment (with information about treatment either lacking or concealed by the patient), or renal sodium loss (salt-losing nephritis, congenital or acquired tubulopathy, cerebral salt-wasting syndrome).
b) In patients with kidney disease and those using diuretics, determination of the cause of hyponatremia based on UNa and ECF water content may be unreliable. Because in such patients all causes of hypotonic hyponatremia are possible, differential diagnosis should be based on the available clinical data and history.
TreatmentTop
1. Management depends on the severity of hyponatremia, its duration, clinical features (cerebral edema, abnormalities of volume status), and risk of neurologic complications.
2. Symptomatic hyponatremia (ie, associated with cerebral edema) always requires immediate treatment, even if serum [Na+] is 125 to 129 mmol/L.
3. In patients with asymptomatic hyponatremia, start by identifying the cause. Treatment is aimed at achieving a slow increase in serum [Na+] up to 130 mmol/L (see below), with a maximum rise of 8 mmol/L per day.Evidence 1Strong recommendation (benefits clearly outweigh downsides; right action for all or almost all patients). Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to the risk of bias from the observational nature of supporting evidence. Verbalis JG, Goldsmith SR, Greenberg A, Schrier RW, Sterns RH. Hyponatremia treatment guidelines 2007: expert panel recommendations. Am J Med. 2007 Nov;120(11 Suppl 1):S1-21. PMID: 17981159.
4. Subsequent measurements of serum [Na+] should always be performed using the same assay.
5. The longer hyponatremia has been developing, the slower it should be corrected. Chronic hyponatremia that is asymptomatic or associated with minor neurologic symptoms should be corrected very slowly. Documented acute hyponatremia (<48 h) may be corrected relatively rapidly.
6. Stop all IV fluids unless they are essential and discontinue all drugs that may contribute to the development of hyponatremia.
7. Try to control the cause of hyponatremia (if possible) and correct coexisting potassium disturbances (hypokalemia is frequent).
8. Patients with chronic hyponatremia and serum [Na+] ≤120 mmol/L are at risk of ODS if sodium levels are increased too quickly. In such cases the rate of serum sodium increase should be 4 to 8 mmol/L/d and should not be >10 mmol/L over any 24–hour period. In patients with risk factors for ODS (hyponatremia ≤105 mmol/L, coexisting hypokalemia, alcohol use disorder, malnutrition, female sex, advanced liver disease), the rate of serum sodium increase should be 4 to 6 mmol/L/d and should not be >8 mmol/L over 24 hours.
9. Special caution is necessary when correcting severe hyponatremia ([Na+] <120 mmol/L) caused by a transient impairment of renal free water excretion (SIAD; hyponatremia with hypovolemia, particularly caused by thiazide diuretics; aldosterone or cortisol deficiency). In such patients resolution of the cause of hyponatremia may lead to a rapid increase in free water clearance (with a decrease in urine specific gravity <1.009) and a dangerously rapid increase in serum sodium levels potentially leading to ODS (see below). Monitor urine output; values >100 mL/h indicate an increase in renal free water excretion. If the serum sodium level reaches the recommended safe range (see above), discontinue treatment aimed at increasing sodium concentration and correct water loss. In the case of a too rapid increase in serum sodium levels (exceeding the recommended safe range), reduce serum [Na+] using a 5% glucose (dextrose) infusion at a rate of, for example, 10 mL/kg over 1 hour or 3 mL/kg/h until a safe serum sodium level is achieved. To prevent further water loss and progressive hypernatremia, administer IV or subcutaneous desmopressin 2 to 4 microg every 8 hours.Evidence 2Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better in some patients). Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness (majority of evidence coming from animal studies). Sterns RH, Thomas DJ, Herndon RM. Brain dehydration and neurologic deterioration after rapid correction of hyponatremia. Kidney Int. 1989 Jan;35(1):69-75. PMID: 2709662. Verbalis JG, Baldwin EF, Robinson AG. Osmotic regulation of plasma vasopressin and oxytocin after sustained hyponatremia. Am J Physiol. 1986 Mar;250(3 Pt 2):R444-51. PMID: 3953853. Desmopressin requires careful monitoring and more intense/experienced milieu use. The advantage of a proactive, reactive, or rescue desmopressin use strategy is not clear.Evidence 3Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to risk of bias and imprecision. MacMillan TE, Tang T, Cavalcanti RB. Desmopressin to Prevent Rapid Sodium Correction in Severe Hyponatremia: A Systematic Review. Am J Med. 2015 Dec;128(12):1362.e15-24. doi: 10.1016/j.amjmed.2015.04.040. Epub 2015 May 30. doi: 10.1016/j.amjmed.2015.04.040. PMID: 26031887.
1. The target serum [Na+] during pharmacotherapy is 130 mmol/L. After reaching the target value, try to normalize serum sodium levels using water restriction and a diet with normal sodium and protein contents.
2. NaCl solutions: Usually 0.9% or 3%.
To estimate the change in serum [Na+] after infusion of 1 L of NaCl solution, use the following formula:
| ∆[Na+] = | [Na+]inf – [Na+]ser |
| TBW + 1 |
Where: ∆[Na+], change in sodium concentration (mmol/L); [Na+]inf, sodium concentration in administered solution (mmol/L) (eg, 513 mmol/L in a 3% NaCl solution); [Na+]ser, current serum [Na+] (mmol/L); TBW, estimated total body water volume expressed in liters (in adults assumed to be 0.6 [men] or 0.5 [women] of body weight; in individuals aged ≥65 years, 0.5 and 0.45, respectively).
Note: This is an expected serum [Na+] increase from baseline after the administration of 1 L of NaCl solution. If the calculated increase is 10 mmol/L and the target increase rate is 1 mmol/L/h, administer 100 mL of the (hypertonic) solution over 1 hour. Measure serum [Na+] and calculate the change in serum [Na+] again (using the current serum [Na+]!) to avoid a too rapid correction of hyponatremia. Note that in many cases the actual increase in serum sodium levels is higher than values estimated using the formula.
In the case of simultaneous correction of hyponatremia and hypokalemia, one may use the following modified formula that takes into account the amount of administered potassium, which also contributes to the increase in serum [Na+]:
| ∆[Na+] = | ([Na+]inf + [K+]inf) – [Na+]ser |
| TBW + 1 |
Where: ∆[Na+], change in sodium concentration (mmol/L); [Na+]inf, sodium concentration in the administered solution (mmol/L); [K+]inf, potassium concentration in the infused solution (mmol/L); [Na+]ser, current serum [Na+] (mmol/L); TBW, estimated total body water volume expressed in liters (see above).
3. Oral solutes: Oral NaCl tablets, in addition to free water restriction, can be administered to promote free water diuresis and increase in serum sodium levels in patients with SIAD. The usual dose is 2 to 6 g (split into bid dosing). Oral urea can also be used in this situation by giving 15 to 60 g/d (0.25-0.5 g/kg/d) in several divided doses. The unpleasant bitter taste of urea can be improved by adding sweeteners.
4. Vasopressin receptor antagonists (vaptans): Blockade of the V2 receptor will produce a selective free water diuresis and thus correct hyponatremia. This approach can be considered in patients with increased or normal ECF water content but should be avoided in patients with decreased ECF water content because of the risk of further volume depletion. Their use should also be avoided in patients with liver disease due to the risk of liver injury.Evidence 4Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to the risk of bias from indirectness (selective patient population in available randomized controlled trials). Schrier RW, Gross P, Gheorghiade M, et al; SALT Investigators. Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N Engl J Med. 2006 Nov 16;355(20):2099-112. Epub 2006 Nov 14. PMID: 17105757.
1. Chronic or acute hyponatremia with severe symptoms of cerebral edema (vomiting, somnolence, seizures, coma): The goal of treatment is a rapid increase in serum [Na+] by ~5 mmol/L. In the first hour of treatment you may administer, for example, 150 mL of 3% NaCl IV over 20 minutes; the dose may be repeated twice if necessary. It has been suggested that both rapid intermittent bolus (RIB) strategy described above and slow continuous infusion (SCI) strategy (0.5-1.0 ml/kg/h infusion) are effective and safe; however, the RIB strategy is preferred due to its efficacy in achieving the target within 1 h).Evidence 5Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness. Baek SH, Jo YH, Ahn S, Medina-Liabres K, Oh YK, Lee JB, Kim S. Risk of Overcorrection in Rapid Intermittent Bolus vs Slow Continuous Infusion Therapies of Hypertonic Saline for Patients With Symptomatic Hyponatremia: The SALSA Randomized Clinical Trial. JAMA Intern Med. 2021 Jan 1;181(1):81-92. doi: 10.1001/jamainternmed.2020.5519. PMID: 33104189; PMCID: PMC7589081. After the administration of each dose, measure serum [Na+]. If symptoms of cerebral edema have resolved following an increase in serum [Na+] by 5 mmol/L over 1 hour, discontinue 3% NaCl and start treatment of the underlying condition, trying to at least maintain the achieved sodium level and prevent a further serum [Na+] increase from exceeding safe daily ranges (see above). In case of no improvement of symptoms after an increase in serum [Na+] by 5 mmol/L over 1 hour, continue the administration of 3% NaCl. The goal of treatment is an increase in serum [Na+] by 1 mmol/L during every subsequent hour. Calculate the volumes of subsequent doses using the formula above. Discontinue 3% NaCl in case of clinical improvement, an increase in serum [Na+] by 10 mmol/L compared with baseline, or upon reaching serum [Na+] of 130 mmol/L.
Neurologic symptoms persisting after an increase in serum [Na+] by 10 mmol/L compared with baseline or after reaching a serum [Na+] of 130 mmol/L indicate causes other than cerebral edema due to hyponatremia.
If 3% NaCl is unavailable, a rescue treatment that may be effective in patients with hyponatremia and features of cerebral edema is the administration of 100 to 200 mL of 20% mannitol IV.
2. Chronic or acute hyponatremia with moderate symptoms of cerebral edema (nausea without vomiting, confusion, headache): Immediately administer 150 mL of 3% NaCl IV over 20 minutes followed by NaCl solution to increase serum [Na+] by 5 to 10 mmol/L over 24 hours. Start treatment of the underlying condition and administer NaCl solution to achieve a serum [Na+] of 130 mmol/L while maintaining the serum sodium increase in the safe daily range (see above).
3. Acute hyponatremia without symptoms of cerebral edema: If possible, discontinue the administration of fluids and drugs that may contribute to hyponatremia, identify the cause of hyponatremia, and start treatment of the underlying condition. In patients with a serum sodium decrease >10 mmol/L, you may administer a single dose of 150 mL of 3% NaCl IV over 20 minutes to prevent a further decrease in serum [Na+] and reduce the risk of cerebral edema.
4. Chronic hyponatremia without symptoms of cerebral edema: Treat hyponatremia according to the general rules (see General Measures, above). Before starting treatment, assess volume status.
1) In patients with hypovolemia, administer a balanced crystalloid solution (eg, lactate Ringer solution) 0.5 to 1 mL/kg/h as IV infusion until hypovolemia is corrected. If serum [Na+] remains <130 mmol/L, manage the patient according to the general rules of hyponatremia treatment. Note that there is a risk of a rapid increase in free water clearance and a dangerous rapid increase in serum [Na+] once hypovolemia has been corrected.
2) In patients with hypervolemia, do not start treatment aimed only at correcting hyponatremia if it is mild to moderate. Treatment of the underlying condition (eg, HF, cirrhosis, nephrotic syndrome, polydipsia) is of key importance. Fluid restriction may prevent a further increase in ECF volume.
3) In patients with euvolemia, treat the underlying condition. Manage patients with moderate to severe hyponatremia according to the general rules. Note that there is a risk of a rapid increase in free water clearance and a dangerous rapid increase in serum [Na+] after the resolution of the cause of hyponatremia (eg, treatment with glucocorticoids or mineralocorticoids, resolution of the cause of SIAD).
Management of Hyponatremia of Known Etiology
Always follow the general rules of hyponatremia treatment (see General Measures, above).
1. SIAD: see Syndrome of Inappropriate Antidiuresis.
2. HF causes chronic hyponatremia. Treatment includes fluid restriction and use of a loop diuretic in case of water overload.
3. Hyponatremia caused by thiazide diuretics is almost always chronic. Discontinuation of the thiazide diuretic and normalization of volume status may lead to a rapid increase in free water clearance and a rapid increase in serum [Na+]. It is important to avoid a too rapid increase in serum [Na+] (see General Measures, above).
4. Hyponatremia caused by mineralocorticoid deficiency, glucocorticoid deficiency, or both: These conditions usually cause chronic hyponatremia with hypovolemia (aldosterone deficiency) or with euvolemia (cortisol deficiency). Correction of hypovolemia or starting hormone replacement therapy may lead to rapid increases in free water clearance and in serum [Na+]. It is important to avoid a too rapid increase in serum [Na+] (see General Measures, above).
5. Hyponatremia in patients with cirrhosis is usually chronic. Increasing serum [Na+] requires restriction of water intake to a volume lower than the daily urine output (usually <750 mL/d). Urine output is most effectively increased by using a loop diuretic in combination with spironolactone; watch for the effect on renal function.
6. Hyponatremia caused by prolonged strenuous exercise is acute and associated with neurologic features of cerebral edema that usually develop after ending the exercise. It is a specific type of transient SIAD. Patients with neurologic symptoms should be managed as in the case of cerebral edema (administer 150 mL of 3% NaCl IV over 20 min; this may be repeated twice when necessary). Water diuresis that starts after the exercise leads to a rapid normalization of serum [Na+]. Prevention of this type of hyponatremia is based on drinking fluids during exercise only in case of thirst and in volumes ≤400 to 800 mL/h.
7. Cerebral salt-wasting syndrome is a rare condition that develops in patients with intracranial pathology (eg, subarachnoid hemorrhage). Typical features include hypotonic hyponatremia, very high urine sodium levels, low serum uric acid levels, orthostatic hypotension, and low central venous pressure. Urine output is high. Treat hyponatremia according to the general rules and correct sodium and water deficits.
ComplicationsTop
ODS is a potentially life-threatening complication that may occur in the course of treatment of chronic hyponatremia, especially with rapid correction (defined variably, eg, as an increase >8 mmol/L over 24 h). A large retrospective observational study of >20,000 patients admitted with hyponatremia revealed that ~17% of all patients had rapid correction of hyponatremia, and 0.05% developed ODS.Evidence 6Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to observational data and indirectness. MacMillan TH, Shin S, Topf J, et al. Osmotic Demyelination Syndrome in Patients Hospitalized with Hyponatremia. NEJM Evid. 2023 Apr;2(4):EVIDoa2200215. doi: 10.1056/EVIDoa2200215. Epub 2023 Mar 23. PMID: 38320046. Clinical manifestations develop over several days and include rapidly developing tetraplegia, pseudobulbar palsy, seizures, and coma. The condition may be fatal.
PrognosisTop
The prognosis in patients with severe hyponatremia causing cerebral edema and with ODS is uncertain; these conditions may cause permanent brain damage. In other patients, the prognosis depends on the underlying condition.
FiguresTop
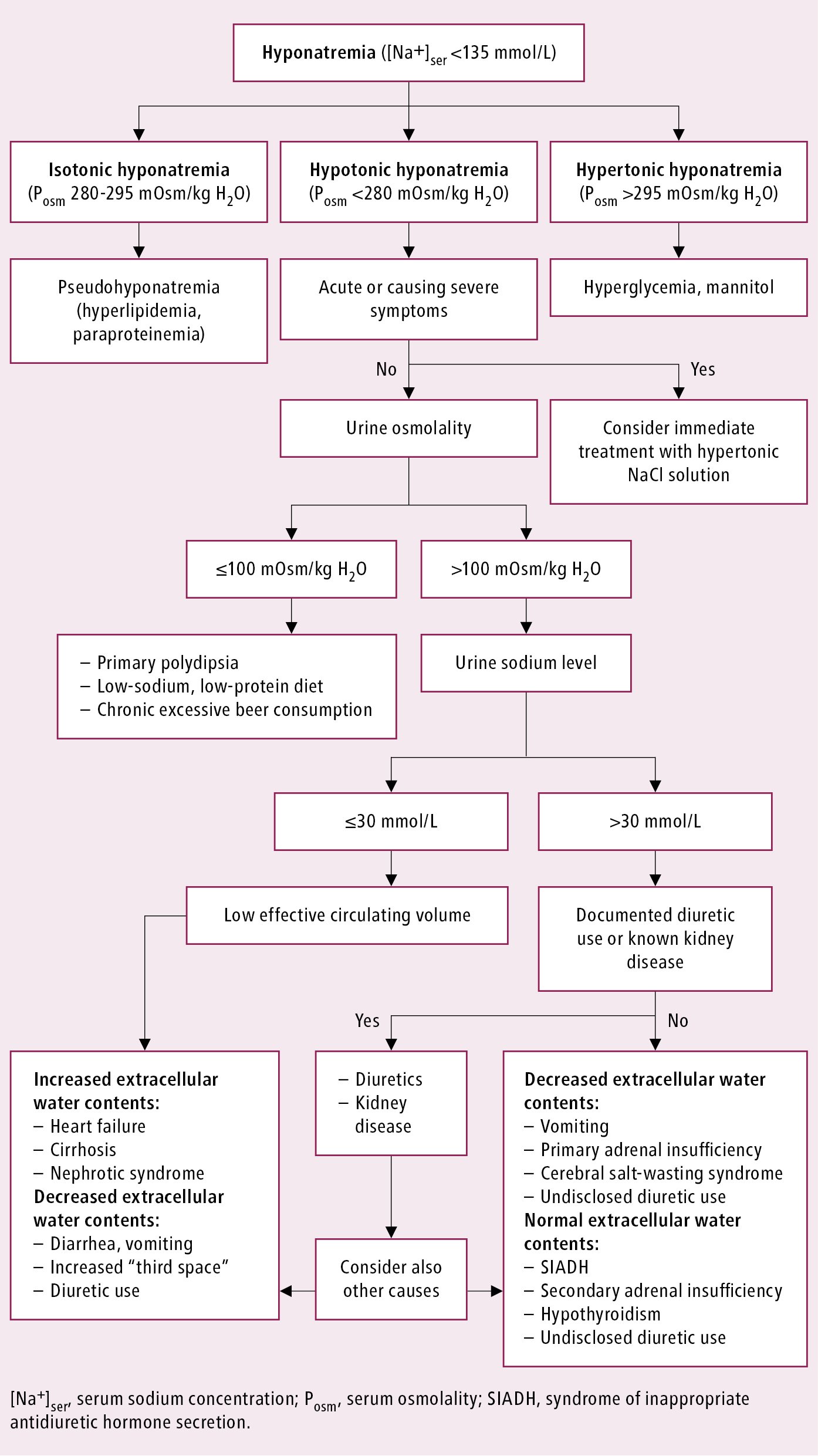
Figure 5.2-1. Diagnostic algorithm in hyponatremia. Adapted from Eur J Endocrinol. 2014;170(3):G1-47.