Glikson M, Nielsen JC, Kronborg MB, et al; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021 Sep 14;42(35):3427-3520. doi: 10.1093/eurheartj/ehab364. Erratum in: Eur Heart J. 2022 May 1;43(17):1651. PMID: 34455430.
Cronin EM, Bogun FM, Maury P, et al; ESC Scientific Document Group. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace. 2019 Aug 1;21(8):1143-1144. doi: 10.1093/europace/euz132. Erratum in: Europace. 2019 Aug 1;21(8):1144. Erratum in: J Arrhythm. 2020 Jan 12;36(1):214. Erratum in: Europace. 2020 Mar 1;22(3):505. PMID: 31075787; PMCID: PMC7967791.
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2018 Sep 25;138(13):e272-e391. doi: 10.1161/CIR.0000000000000549. Erratum in: Circulation. 2018 Sep 25;138(13):e419-e420. PMID: 29084731.
Bennett M, Parkash R, Nery P, et al. Canadian Cardiovascular Society/Canadian Heart Rhythm Society 2016 Implantable Cardioverter-Defibrillator Guidelines. Can J Cardiol. 2017 Feb;33(2):174-188. doi: 10.1016/j.cjca.2016.09.009. Epub 2016 Oct 6. PMID: 28034580.
Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013 Dec;10(12):1932-63. doi: 10.1016/j.hrthm.2013.05.014. Epub 2013 Aug 30. Review. PubMed PMID: 24011539.
Postema PG, Wolpert C, Amin AS, et al. Drugs and Brugada syndrome patients: review of the literature, recommendations, and an up-to-date website (www.brugadadrugs.org). Heart Rhythm. 2009;6(9):1335-1341. doi:10.1016/j.hrthm.2009.07.002
Definition and EtiologyTop
Brugada syndrome (BrS) is a rare autosomal dominant disease that is 8 times more prevalent in men than in women; it is also more frequent in eastern Asia, where it affects 0.05% to 0.1% of the general population. Disease onset is usually between the age of 20 and 40 years but sometimes may occur earlier, particularly in patients with malignant arrhythmias.
Clinical FeaturesTop
Key clinical features include syncope caused by fast polymorphic ventricular tachycardia (VT), cardiac arrest, or sudden cardiac death (SCD). SCD typically occurs at night. Syncope may be a preliminary symptom.
DiagnosisTop
Electrocardiography (ECG) (Figure 3.4-1) during sinus rhythm has a distinctive pattern and is characterized by an ST-segment elevation of ≥2 mm with a negative T wave in ≥1 right precordial lead (V1-V3) positioned in the fourth, third, or second intercostal space. This Brugada ECG pattern can be transient and is typically apparent in patients with high fever. Sodium channel blocker antiarrhythmic drugs (flecainide, procainamide, ajmaline) can unmask the pattern.
There are 3 described ECG patterns but only the type 1 morphology is diagnostic of BrS. In case of clinical suspicion of BrS in the absence of a spontaneous type 1 ST-segment elevation, a pharmacologic challenge using a sodium channel blocker is recommended. When a type 1 ST-segment elevation is unmasked using a sodium channel blocker, the diagnosis of BrS should require that the patient also present with 1 of the following: documented ventricular fibrillation (VF) or polymorphic VT, syncope of a probable arrhythmic cause, family history of SCD at <45 years with negative autopsy, coved-type ECG in family members, or nocturnal gasping. The diagnosis of BrS can be challenging.
Differential diagnosis of right precordial ST-segment elevation includes atypical right bundle branch block, early repolarization, acute myocardial ischemia, arrhythmogenic right ventricular cardiomyopathy, and pectus excavatum.
TreatmentTop
Classification of antiarrhythmic drugs: see Table 3.4-1.
Antiarrhythmic agents: see Table 3.4-2.
1. Implantable cardioverter-defibrillator (ICD) is the first-line therapy for patients with BrS presenting with aborted SCD or documented VT or VF. ICDs can be used prophylactically in BrS patients with a spontaneous manifest ECG pattern (type 1) and unexplained syncope with cardiac features.
2. Asymptomatic patients with a Brugada ECG pattern (type 1), either spontaneous or induced by sodium channel blockers, can be closely followed without an ICD after seeking expert advice.
3. Sodium blockers should be avoided; a full list of medications can be found at brugadadrugs.org.
4. Quinidine may be considered, if available, in BrS patients presenting with electrical storm or frequent ICD shocks. It may also be useful in patients who qualify for an ICD but the device is unavailable, refused, or contraindicated. Isoproterenol can be useful in the case of a Brugada VT/VF storm.
FiguresTop
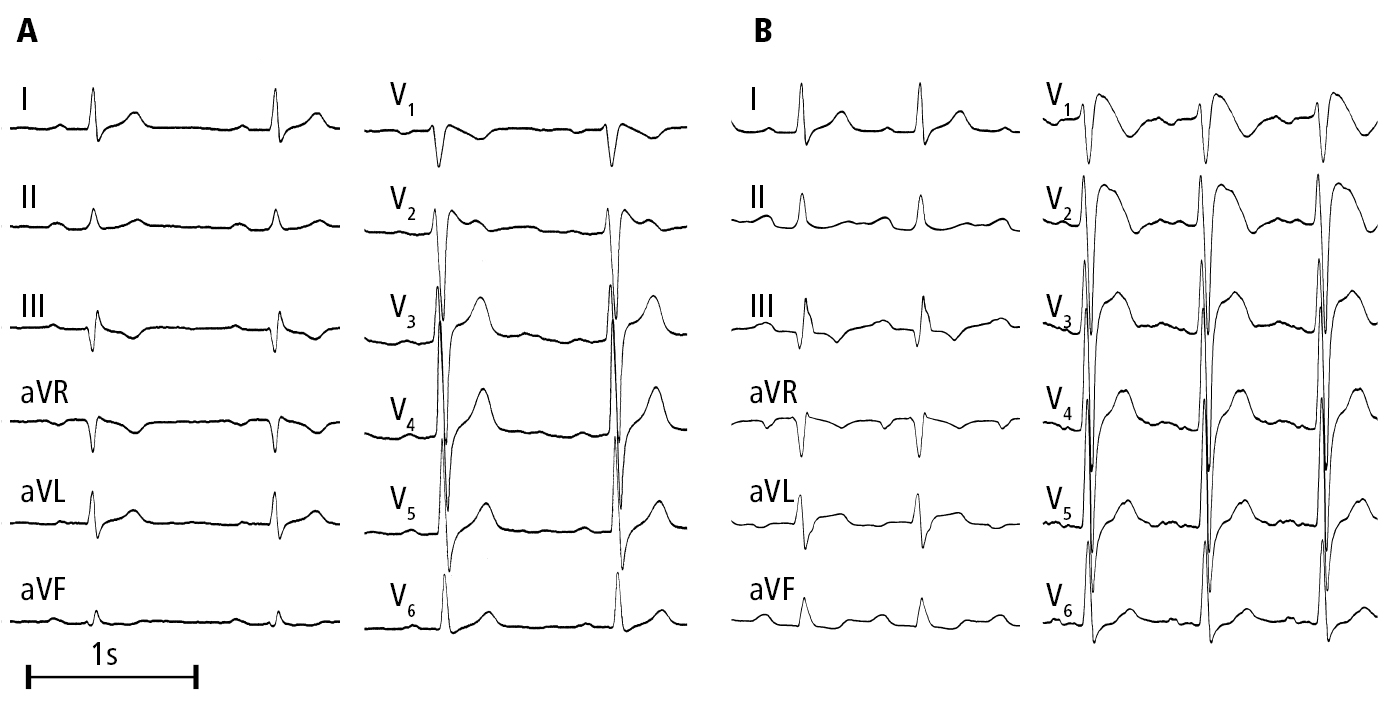
Figure 3.4-1. Electrocardiography (ECG) of a patient with Brugada syndrome: A, nearly undetectable changes; B, a typical ECG pattern 9 days later. Figure courtesy of Dr Andrzej Stanke.