Van Gelder IC, Rienstra M, Bunting KV, et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2024;45(36):3314-3414. doi:10.1093/eurheartj/ehae176
Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines [published correction appears in Circulation. 2024 Jan 2;149(1):e167. doi: 10.1161/CIR.0000000000001207.] [published correction appears in Circulation. 2024 Feb 27;149(9):e936. doi: 10.1161/CIR.0000000000001218.] [published correction appears in Circulation. 2024 Jun 11;149(24):e1413. doi: 10.1161/CIR.0000000000001263.]. Circulation. 2024;149(1):e1-e156. doi:10.1161/CIR.0000000000001193
Glikson M, Nielsen JC, Kronborg MB, et al; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021 Sep 14;42(35):3427-3520. doi: 10.1093/eurheartj/ehab364. PMID: 34455430.
Andrade JG, Aguilar M, Atzema C, et al. The 2020 Canadian Cardiovascular Society/Canadian Heart Rhythm Society Comprehensive Guidelines for the Management of Atrial Fibrillation. Can J Cardiol. 2020 Dec;36(12):1847-1948. doi:10.1016/j.cjca.2020.09.001. Epub 2020 Oct 22. PMID: 33191198.
Brugada J, Katritsis DG, Arbelo E, et al; ESC Scientific Document Group. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia: The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2020 Feb 1;41(5):655-720. doi: 10.1093/eurheartj/ehz467. Erratum in: Eur Heart J. 2020 Nov 21;41(44):4258. PMID: 31504425.
January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019 Jul 9;74(1):104-132. doi: 10.1016/j.jacc.2019.01.011. Epub 2019 Jan 28. Erratum in: J Am Coll Cardiol. 2019 Jul 30;74(4):599. PMID: 30703431.
Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2019 Sep;16(9):e128-e226. doi: 10.1016/j.hrthm.2018.10.037. Epub 2018 Nov 6. PMID: 30412778.
January CT, Wann LS, Alpert JS, et al; ACC/AHA Task Force Members. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014 Dec 2;130(23):e199-267. doi: 10.1161/CIR.0000000000000041. Epub 2014 Mar 28. Erratum in: Circulation. 2014 Dec 2;130(23):e272-4. PMID: 24682347; PMCID: PMC4676081.
Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013 Dec;10(12):1932-63. doi: 10.1016/j.hrthm.2013.05.014. Epub 2013 Aug 30. Review. PMID: 24011539.
Pediatric and Congenital Electrophysiology Society (PACES); Heart Rhythm Society (HRS); American College of Cardiology Foundation (ACCF); American Heart Association (AHA); American Academy of Pediatrics (AAP); Canadian Heart Rhythm Society (CHRS), Cohen MI, Triedman JK, Cannon BC, et al. PACES/HRS expert consensus statement on the management of the asymptomatic young patient with a Wolff-Parkinson-White (WPW, ventricular preexcitation) electrocardiographic pattern: developed in partnership between the Pediatric and Congenital Electrophysiology Society (PACES) and the Heart Rhythm Society (HRS). Endorsed by the governing bodies of PACES, HRS, the American College of Cardiology Foundation (ACCF), the American Heart Association (AHA), the American Academy of Pediatrics (AAP), and the Canadian Heart Rhythm Society (CHRS). Heart Rhythm. 2012 Jun;9(6):1006-24. doi: 10.1016/j.hrthm.2012.03.050. Epub 2012 May 10. PMID: 22579340.
Definition, Etiology, PathogenesisTop
Atrioventricular nodal reentrant tachycardia (AVNRT) is a paroxysmal tachycardia that occurs in patients with dual atrioventricular (AV) node physiology, as they have both a fast nodal pathway with a longer refractory period and a slow nodal pathway with a shorter refractory period. It is most commonly observed in individuals with no underlying structural heart disease.
Types of AVNRT:
1) Typical and most common type of AVNRT: Anterograde conduction (from the atrium to the ventricle) proceeds over the slow pathway and retrograde conduction (from the ventricle to the atrium) proceeds over the fast pathway (slow-fast AVNRT).
2) Atypical AVNRT: Anterograde conduction proceeds over the fast pathway and retrograde conduction proceeds over the slow pathway (fast-slow AVNRT).
Clinical Features and Natural HistoryTop
AVNRT usually occurs in young patients, causing paroxysmal palpitations that abruptly start and stop. The palpitations are usually relatively well tolerated, as no concomitant structural heart disease is found and the heart rates are typically ≤170 to 180 beats/min. Patients may describe a sensation of rapid regular pounding in the neck during tachycardia. The attacks may be frequent (up to several a day) and may require emergency care.
DiagnosisTop
Electrocardiography (ECG) (Figure 3.4-1): Typical AVNRT is characterized by the absence of evident P waves, which are hidden in or present immediately after the QRS complex (short RP interval) but may distort the terminal portion of the QRS by mimicking an S wave in the inferior leads or an r wave in lead V1. In atypical AVNRT the RP interval is long (RP interval > PR interval). In both typical and atypical AVNRTs the P waves are negative in the inferior leads.
TreatmentTop
Classification of antiarrhythmic drugs: see Table 3.4-1.
Antiarrhythmic agents: see Table 3.4-2.
1. Termination of an AVNRT attack:
1) Vagal maneuvers (eg, Valsalva,Evidence 1Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision. Smith GD, Fry MM, Taylor D, Morgans A, Cantwell K. Effectiveness of the Valsalva Manoeuvre for reversion of supraventricular tachycardia. Cochrane Database Syst Rev. 2015 Feb 18;(2):CD009502. doi: 10.1002/14651858.CD009502.pub3. Review. PubMed PMID: 25922864. carotid massage, and face immersion in cold water) should be initiated to terminate the arrhythmia or to modify AV conduction.
2) IV adenosine as a bolus of 6 mg. If not effective, 12 or 18 mg can be given after 1 to 2 minutes.
3) IV beta-blockers, diltiazem, or verapamil are a reasonable option in stable patients.
4) Direct current cardioversion should be performed for acute treatment in hemodynamically unstable patients.
2. Recurrence prevention:
1) In patients with frequently recurring AVNRT attacks who prefer long-term oral treatment to ablation, use diltiazem, verapamil, or a beta‑blocker.
2) In patients with no structural heart disease who do not respond to drugs that inhibit AV node conduction (see above), use flecainide or propafenone.
3) In minimally symptomatic patients with AVNRT, clinical follow-up without pharmacologic therapy or ablation is reasonable.
4) In patients with poorly tolerated AVNRT, recurrent attacks, and significant symptoms, as well as in those with mild and well-tolerated symptoms who wish to achieve a complete cure of AVNRT, catheter ablation of the slow pathway is indicated. This is the most successful treatment method, although associated with a low risk (0.5%-1%) of AV block requiring pacemaker implantation.
FiguresTop
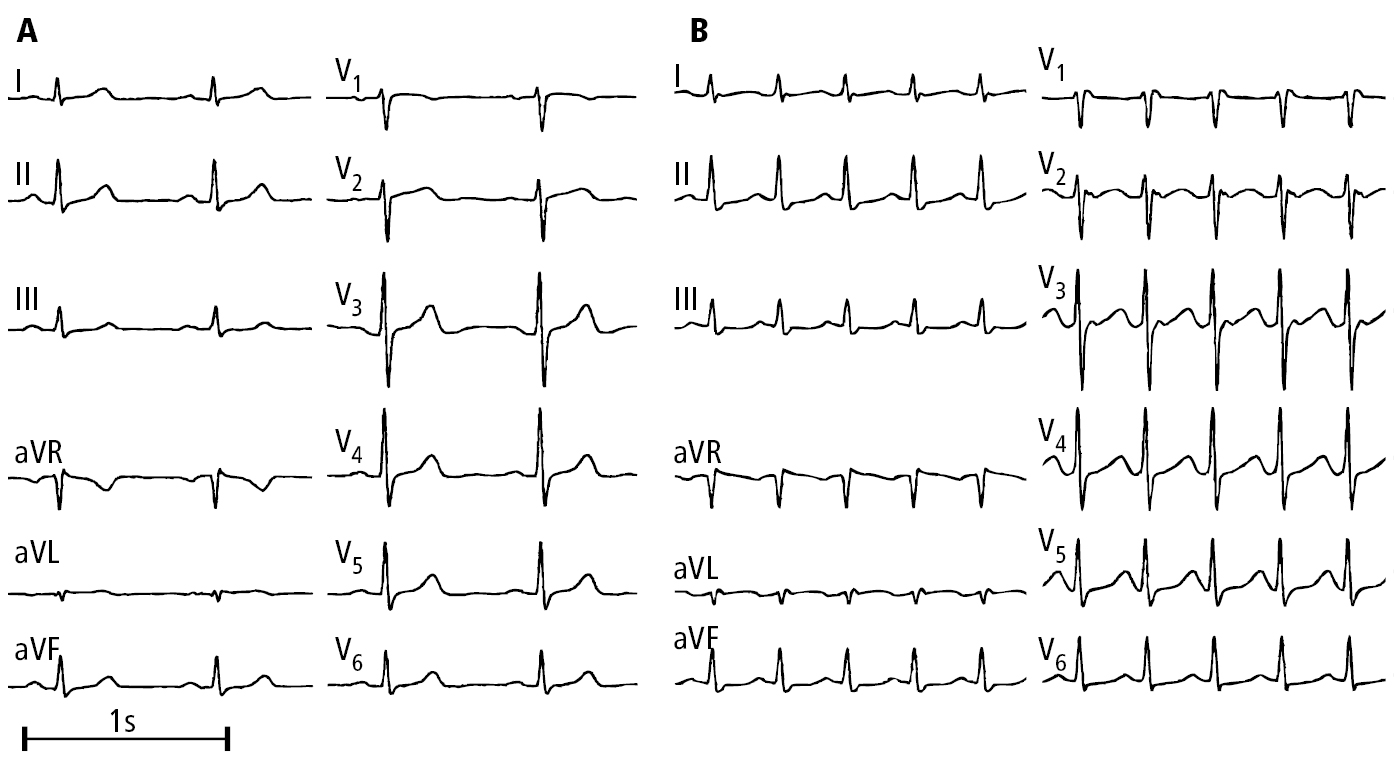
Figure 3.4-1. Electrocardiography (ECG) of a patient with paroxysmal atrioventricular nodal reentrant tachycardia (AVNRT): A, sinus rhythm; B, tachycardia, pseudo r’ wave (P wave) in lead V1. Figure courtesy of Dr Andrzej Stanke.