Van Gelder IC, Rienstra M, Bunting KV, et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2024;45(36):3314-3414. doi:10.1093/eurheartj/ehae176
Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines [published correction appears in Circulation. 2024 Jan 2;149(1):e167. doi: 10.1161/CIR.0000000000001207.] [published correction appears in Circulation. 2024 Feb 27;149(9):e936. doi: 10.1161/CIR.0000000000001218.] [published correction appears in Circulation. 2024 Jun 11;149(24):e1413. doi: 10.1161/CIR.0000000000001263.]. Circulation. 2024;149(1):e1-e156. doi:10.1161/CIR.0000000000001193
Glikson M, Nielsen JC, Kronborg MB, et al; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021 Sep 14;42(35):3427-3520. doi: 10.1093/eurheartj/ehab364. PMID: 34455430.
Andrade JG, Aguilar M, Atzema C, et al. The 2020 Canadian Cardiovascular Society/Canadian Heart Rhythm Society Comprehensive Guidelines for the Management of Atrial Fibrillation. Can J Cardiol. 2020 Dec;36(12):1847-1948. doi:10.1016/j.cjca.2020.09.001. Epub 2020 Oct 22. PMID: 33191198.
Brugada J, Katritsis DG, Arbelo E, et al; ESC Scientific Document Group. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia: The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2020 Feb 1;41(5):655-720. doi: 10.1093/eurheartj/ehz467. Erratum in: Eur Heart J. 2020 Nov 21;41(44):4258. PMID: 31504425.
January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019 Jul 9;74(1):104-132. doi: 10.1016/j.jacc.2019.01.011. Epub 2019 Jan 28. Erratum in: J Am Coll Cardiol. 2019 Jul 30;74(4):599. PMID: 30703431.
Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2019 Sep;16(9):e128-e226. doi: 10.1016/j.hrthm.2018.10.037. Epub 2018 Nov 6. PMID: 30412778.
January CT, Wann LS, Alpert JS, et al; ACC/AHA Task Force Members. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014 Dec 2;130(23):e199-267. doi: 10.1161/CIR.0000000000000041. Epub 2014 Mar 28. Erratum in: Circulation. 2014 Dec 2;130(23):e272-4. PMID: 24682347; PMCID: PMC4676081.
Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013 Dec;10(12):1932-63. doi: 10.1016/j.hrthm.2013.05.014. Epub 2013 Aug 30. Review. PMID: 24011539.
Pediatric and Congenital Electrophysiology Society (PACES); Heart Rhythm Society (HRS); American College of Cardiology Foundation (ACCF); American Heart Association (AHA); American Academy of Pediatrics (AAP); Canadian Heart Rhythm Society (CHRS), Cohen MI, Triedman JK, Cannon BC, et al. PACES/HRS expert consensus statement on the management of the asymptomatic young patient with a Wolff-Parkinson-White (WPW, ventricular preexcitation) electrocardiographic pattern: developed in partnership between the Pediatric and Congenital Electrophysiology Society (PACES) and the Heart Rhythm Society (HRS). Endorsed by the governing bodies of PACES, HRS, the American College of Cardiology Foundation (ACCF), the American Heart Association (AHA), the American Academy of Pediatrics (AAP), and the Canadian Heart Rhythm Society (CHRS). Heart Rhythm. 2012 Jun;9(6):1006-24. doi: 10.1016/j.hrthm.2012.03.050. Epub 2012 May 10. PMID: 22579340.
Definition, Etiology, PathogenesisTop
Preexcitation syndromes refer to a form of congenital arrhythmias resulting from the presence of accessory pathways, that is, muscle fibers bypassing the physiologic conduction system and causing early activation of a part of the ventricle. The most common type is Wolff-Parkinson-White (WPW) syndrome, which refers to the presence of an accessory pathway in association with supraventricular tachycardia (SVT).
Tachyarrhythmias observed in patients with WPW syndrome:
1) Orthodromic atrioventricular reentrant tachycardia (AVRT) (>85% of patients): A narrow-QRS tachycardia with anterograde conduction (from the atrium to the ventricle) over the atrioventricular (AV) node and retrograde conduction (from the ventricle to the atrium) over the accessory pathway.
2) Antidromic AV tachycardia: A wide-QRS tachycardia with anterograde conduction over the accessory pathway and retrograde conduction over the AV node or another accessory pathway.
3) Preexcited atrial fibrillation (AF): AF with rapid ventricular response, usually with varying degrees of preexcitation (different QRS widths). This may develop in patients with an accessory pathway capable of fast conduction.
Clinical Features and Natural HistoryTop
Symptoms (mainly palpitations) are seen in ~50% of patients with electrocardiographic (ECG) features of preexcitation and usually start during childhood; a new diagnosis of preexcitation in older individuals is rare. The presenting event may be ventricular fibrillation or sometimes syncope requiring hospital admission. Compared with healthy population, the risk of sudden cardiac death is increased particularly in symptomatic patients.
DiagnosisTop
1. ECG (Figure 3.4-10):
1) Features of ventricular preexcitation during sinus rhythm: A shortened PR interval (<0.12 seconds) and a wide QRS with a delta wave in the first portion of the QRS. If preexcitation is not clear, one option is to repeat the ECG during IV administration of adenosine to block the AV node and reveal the accessory pathway (Figure 3.4-11).
2) ECG recorded during SVT:
a) Orthodromic AVRT: A regular narrow QRS with a retrograde P wave usually visible in the first portion of the ST segment (short-RP tachycardia).
b) Antidromic AVRT: A regular wide QRS of a fully preexcited morphology (morphology resembles preexcitation during sinus rhythm but QRS is wider).
c) Preexcited AF: An irregularly irregular rhythm with varying widths of QRS depending on the degree of preexcitation. At times there is a very rapid ventricular response.
2. Electrophysiologic study (EPS) is used to confirm the presence of an accessory pathway, establish the number and location of the pathways, assess their refractory periods, and to induce tachyarrhythmia to confirm the diagnosis.
SVT: see Figure 3.4-2. Narrow-QRS tachycardia: see Figure 3.4-3. Wide-QRS tachycardia: see Figure 3.4-4.
An abnormal QRS shape resulting from preexcitation may mimic myocardial infarction (MI), bundle branch blocks, or ventricular hypertrophy.
TreatmentTop
Termination of SVT:
1) Orthodromic (narrow-QRS) AVRT:
a) Same as for AVNRT (see Atrioventricular Nodal Reentrant Tachycardia).
b) Vagal maneuvers.
c) IV adenosine, diltiazem, verapamil, or beta-blockers can be used.
d) Synchronized cardioversion should be considered in hemodynamically unstable patients and in stable patients when pharmacologic therapy is ineffective or contraindicated.
e) IV ibutilide or IV procainamide is beneficial for acute treatment in patients with preexcited AF. If not available, IV amiodarone may be considered (not recommended by the European Society of Cardiology [ESC]).
2) Antidromic (wide-QRS) AVRT: Administer antiarrhythmic drugs that act on the accessory pathway (eg, procainamide, flecainide, or propafenone, in preference to amiodarone) or perform cardioversion. If preexcited AF has been excluded, a trial of adenosine or nodal blockers is an acceptable choice.
3) Preexcited AF: Adenosine and nodal blockers (calcium antagonists, beta-blockers, digoxin, and likely amiodarone [unless no alternative is available]) should not be used, as they may predispose to rapid ventricular rates and trigger ventricular fibrillation.
1. Patients with asymptomatic preexcitation:
1) EPS is reasonable to evaluate the risk for arrhythmic events. If EPS identifies a high risk for arrhythmic events, catheter ablation is recommended.
2) The finding of abrupt loss of conduction over a manifest pathway during an exercise test or ambulatory monitoring is useful to identify patients at low risk of preexcited AF (the pathway would not be able to conduct at a very high heart rate during AF).
2. In patients with WPW syndrome causing symptomatic but well-tolerated arrhythmia, catheter ablation is considered first-line therapy, as it is highly effective and carries a low risk of complications. Medications are generally stopped after a successful procedure.
3. In patients with AVRT but without preexcitation in resting ECG, oral beta-blockers, diltiazem, or verapamil are indicated for ongoing management. The confirmation of AVRT if preexcitation is not present in ECG during sinus rhythm can only be made with an EPS.
4. In patients with preexcitation and SVT who are not candidates for ablation use flecainide or propafenone to block conduction through the accessory pathway. If not available or contraindicated, amiodarone or sotalol may be also considered.
5. In patients with WPW syndrome causing AF with fast conduction or poorly tolerated AVRT, catheter ablation is highly recommended.
FiguresTop
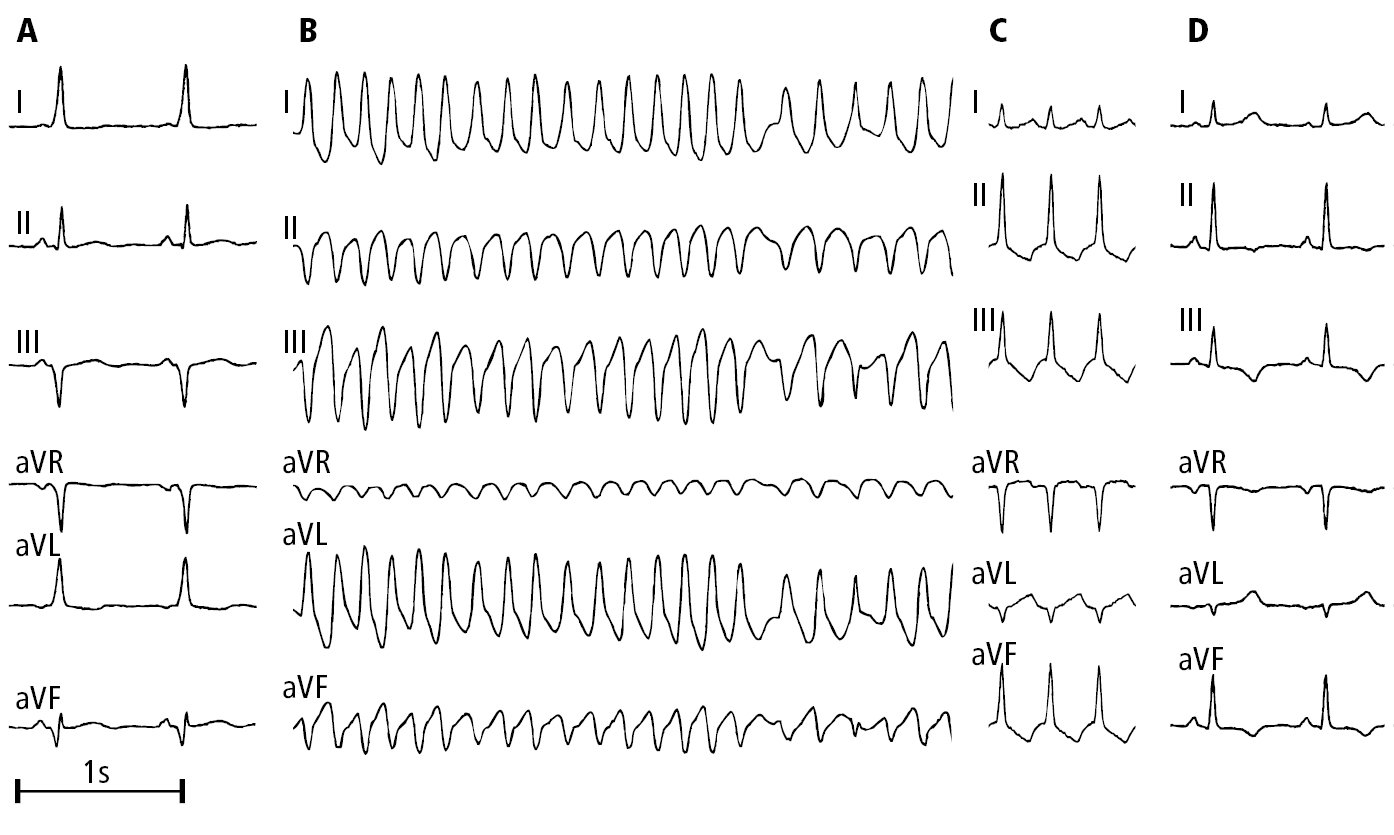
Figure 3.4-10. Electrocardiography (ECG) of a patient with Wolff-Parkinson-White syndrome: A, sinus rhythm (with preexcitation); B, preexcited atrial fibrillation; C, orthodromic atrioventricular reentrant tachycardia (AVRT); D, status post ablation, sinus rhythm without preexcitation. Figure courtesy of Dr Andrzej Stanke.
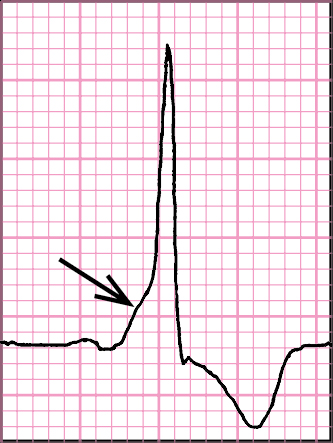
Figure 3.4-11. Preexcitation syndrome: short PR interval, delta wave on the ascending arm of the R wave (arrow), ST segment and T wave discordant with the QRS complex.