Glikson M, Nielsen JC, Kronborg MB, et al; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021 Sep 14;42(35):3427-3520. doi: 10.1093/eurheartj/ehab364. Erratum in: Eur Heart J. 2022 May 1;43(17):1651. PMID: 34455430.
Cronin EM, Bogun FM, Maury P, et al; ESC Scientific Document Group. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace. 2019 Aug 1;21(8):1143-1144. doi: 10.1093/europace/euz132. Erratum in: Europace. 2019 Aug 1;21(8):1144. Erratum in: J Arrhythm. 2020 Jan 12;36(1):214. Erratum in: Europace. 2020 Mar 1;22(3):505. PMID: 31075787; PMCID: PMC7967791.
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2018 Sep 25;138(13):e272-e391. doi: 10.1161/CIR.0000000000000549. Erratum in: Circulation. 2018 Sep 25;138(13):e419-e420. PMID: 29084731.
Bennett M, Parkash R, Nery P, et al. Canadian Cardiovascular Society/Canadian Heart Rhythm Society 2016 Implantable Cardioverter-Defibrillator Guidelines. Can J Cardiol. 2017 Feb;33(2):174-188. doi: 10.1016/j.cjca.2016.09.009. Epub 2016 Oct 6. PMID: 28034580.
Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013 Dec;10(12):1932-63. doi: 10.1016/j.hrthm.2013.05.014. Epub 2013 Aug 30. Review. PubMed PMID: 24011539.
Definition, Etiology, PathogenesisTop
Idiopathic ventricular tachycardias (VTs) primarily include several types of focal arrhythmias (outflow tract VT, fascicular VT, papillary muscle VT) in patients without coronary artery disease (CAD) or structural heart disease. Rarely there may be annular VT. These arrhythmias are idiopathic and generally associated with good prognosis. They may present as frequent premature ventricular contractions (PVCs) or episodes of sustained VT, usually monomorphic.
Clinical Features and Natural HistoryTop
Symptoms range from none (asymptomatic) to paroxysmal palpitations. Symptom severity depends on the hemodynamic significance of the arrhythmia. Patients with very frequent PVCs (>10% of total beats in 24 hours) may develop cardiomyopathy. Symptoms are frequently exacerbated by stress or exercise.
DiagnosisTop
Electrocardiography (ECG):
1) Outflow tract VT can arise from the right ventricular outflow tract or the left ventricular outflow tract. It is the most common type, either in the form of monomorphic PVCs or monomorphic VT. The hallmark is an inferior axis on ECG (positive QRS in the inferior leads; Figure 3.4-11).
2) Fascicular VT: The most common origin is the left posterior fascicle of the left bundle branch. ECG during tachycardia reveals a slightly widened QRS (usually <140 milliseconds, not as wide as in other VTs) with right bundle branch block (RBBB) and a left axis deviation (negative QRS in the inferior leads).
3) Papillary muscle VT: Similar to fascicular VT but with a wider QRS (>140 milliseconds).
Differential diagnosis should include other types of VT or supraventricular tachycardia with aberrancy. It is important to exclude structural heart disease and to analyze QRS morphology during the arrhythmia. VT in arrhythmogenic right ventricular cardiomyopathy can resemble benign right outflow tachycardia; determination of the nature of ventricular arrhythmia in these cases is an evolving field requiring expert input.
TreatmentTop
Classification of antiarrhythmic drugs: see Table 3.4-1.
Antiarrhythmic agents: see Table 3.4-2.
1. Fascicular VT commonly responds to verapamil (IV or oral).
2. When outflow tract VT/PVCs are suspected, beta-blockers, diltiazem, or verapamil should be considered. This type of VT may also respond to class Ic antiarrhythmics.
3. Catheter ablation is indicated in patients with focal PVCs/VT or fascicular VT who do not respond to antiarrhythmic drugs, are not willing to take medications on a long-term basis, or cannot tolerate the drugs.
FiguresTop
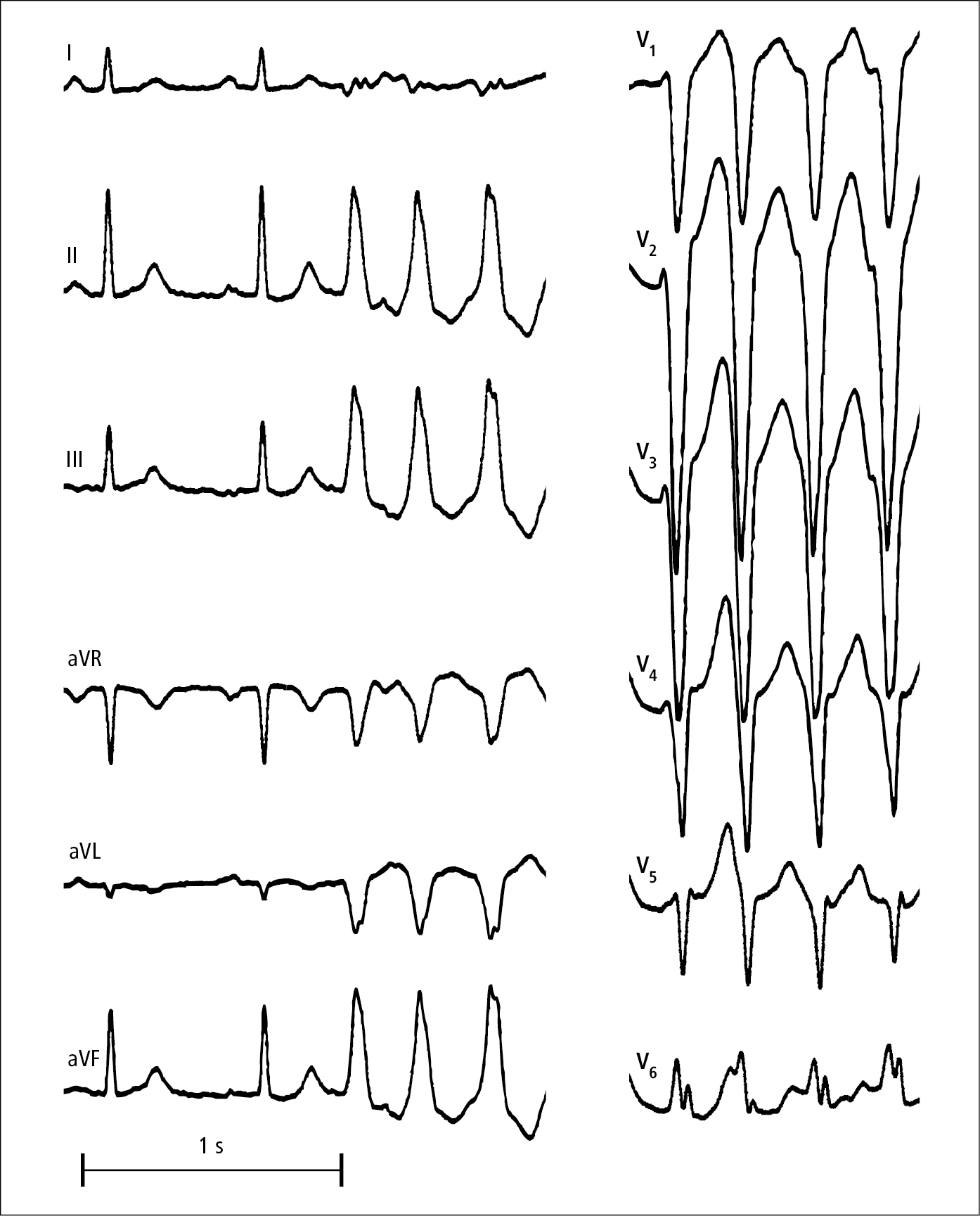
Figure 3.4-11. Episode of monomorphic right ventricular outflow tract tachycardia.