Glikson M, Nielsen JC, Kronborg MB, et al; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021 Sep 14;42(35):3427-3520. doi: 10.1093/eurheartj/ehab364. Erratum in: Eur Heart J. 2022 May 1;43(17):1651. PMID: 34455430.
Cronin EM, Bogun FM, Maury P, et al; ESC Scientific Document Group. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace. 2019 Aug 1;21(8):1143-1144. doi: 10.1093/europace/euz132. Erratum in: Europace. 2019 Aug 1;21(8):1144. Erratum in: J Arrhythm. 2020 Jan 12;36(1):214. Erratum in: Europace. 2020 Mar 1;22(3):505. PMID: 31075787; PMCID: PMC7967791.
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2018 Sep 25;138(13):e272-e391. doi: 10.1161/CIR.0000000000000549. Erratum in: Circulation. 2018 Sep 25;138(13):e419-e420. PMID: 29084731.
Bennett M, Parkash R, Nery P, et al. Canadian Cardiovascular Society/Canadian Heart Rhythm Society 2016 Implantable Cardioverter-Defibrillator Guidelines. Can J Cardiol. 2017 Feb;33(2):174-188. doi: 10.1016/j.cjca.2016.09.009. Epub 2016 Oct 6. PMID: 28034580.
Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013 Dec;10(12):1932-63. doi: 10.1016/j.hrthm.2013.05.014. Epub 2013 Aug 30. Review. PubMed PMID: 24011539.
Definition, Etiology, PathogenesisTop
Patients after myocardial infarction (MI) can develop a myriad of ventricular arrhythmias. Polymorphic ventricular tachycardia (VT) or ventricular fibrillation (VF) can develop in the acute phase of MI or during periods of acute ischemia at a later stage. Scar-related arrhythmia (chronic phase of ischemic cardiomyopathy) is usually manifested as monomorphic VT, either nonsustained (NSVT) or sustained. Sustained monomorphic VT usually develops in patients with more extensive necrosis and depressed left ventricular (LV) function; this type of VT is related to a reentrant circuit within the myocardial scar.
Clinical Features and Natural HistoryTop
NSVT may be asymptomatic. However, sustained VT occurring in this group of patients, particularly during faster rhythms (>150-170 beats/min), may cause significant hemodynamic abnormalities leading to hypotension, chest pain, heart failure, syncope, or cardiac arrest (VT can transform into VF).
DiagnosisTop
Electrocardiography (ECG): see Figure 3.3-1. Polymorphic VT or VF is manifested as a chaotic ventricular rhythm. Sustained monomorphic VT presents as a wide-complex tachycardia and needs to be differentiated from supraventricular tachycardia with aberrancy and from antidromic atrioventricular reentrant tachycardia. The morphology of the VT can help define the origin (myocardial earliest activation point). For example, in a patient with a previous apical MI (the left anterior descending artery [LAD] territory) a monomorphic VT would have predominantly negative QRS in the precordial leads.
TreatmentTop
Classification of antiarrhythmic drugs: see Table 3.4-1.
Antiarrhythmic agents: see Table 3.4-2.
See ST-Segment Elevation Myocardial Infarction (STEMI) and Figure 3.4-12.
1. Optimize ischemic heart disease treatment, including revascularization and treatment of LV dysfunction or heart failure. All patients should receive a beta‑blocker unless contraindicated.
2. Antiarrhythmic medications: Patients who had VT or VF while on beta-blocker therapy may be considered for a trial of amiodarone to prevent arrhythmia recurrence. Although sotalol is less effective, it is still an option for patients who cannot use amiodarone.
3. Catheter ablation of VT was shown to reduce recurrent episodes of VT, particularly in patients already receiving amiodarone.
4. Implantable cardioverter-defibrillator (ICD): This is indicated for secondary prevention of sudden cardiac death (SCD) in patients who have survived VF or VT causing hemodynamic instability unless the episode occurred in the setting of acute ischemia with a treatable cause. The indication as primary prevention (individuals at risk for SCD who have not had an episode yet) includes patients >40 days after MI with an LV ejection fraction ≤30 to 35%. If ICD implantation is not possible despite indications (patient refusal, contraindications, lack of resources), administer amiodarone.
5. Other: For patients with refractory VT surgical endocardial resection of the scarred area or cardiac sympathetic denervation is sometimes proposed (very limited data).
FiguresTop
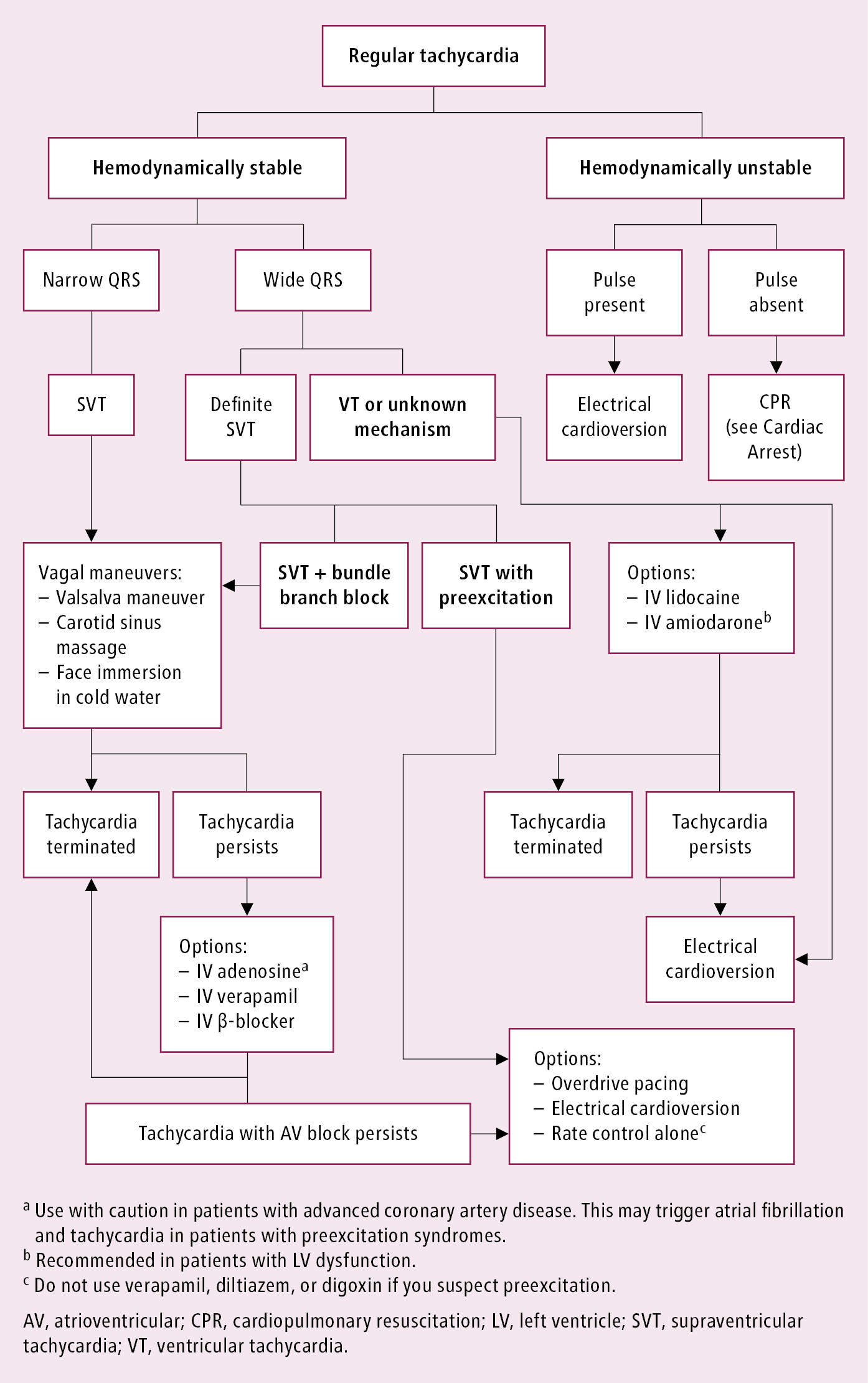
Figure 3.4-12. Acute management of patients with regular tachycardia. Adapted from guidelines by the American College of Cardiology, American Heart Association, and European Society of Cardiology.