Glikson M, Nielsen JC, Kronborg MB, et al; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021 Sep 14;42(35):3427-3520. doi: 10.1093/eurheartj/ehab364. Erratum in: Eur Heart J. 2022 Feb 16;: PMID: 34455430.
Writing Committee Members, Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2019 Sep;16(9):e128-e226. doi: 10.1016/j.hrthm.2018.10.037. Epub 2018 Nov 6. PMID: 30412778.
DefinitionTop
Cardiac conduction system: Figure 3.2-1.
Disorders of automaticity and conduction include sinus node dysfunction, atrioventricular (AV) block, and intraventricular block. Disturbances may occur at one or more levels, may be acute or chronic, and may be sustained or paroxysmal. Bradycardia is classified according to the European Society of Cardiology guidelines as persistent or intermittent (either documented by electrocardiography [ECG] or suspected [undocumented by ECG]).
Clinical FeaturesTop
Clinical manifestations depend mainly on the type and severity of bradycardia, age, presence of structural heart disease, and physical activity. Symptoms may range from reduced exercise tolerance or presyncope to syncope and sudden cardiac death. Symptoms of persistent bradycardia include easy fatigability, fatigue, irritability, concentration impairment, apathy, cognitive impairment, memory impairment, vertigo or dizziness, dyspnea, symptoms of heart failure, and reduced exercise tolerance (chronotropic incompetence). Symptoms of intermittent bradycardia include presyncope, syncope (Adams-Stokes attack), vertigo or dizziness, blurred vision, sudden dyspnea and chest pain unrelated to exercise, and palpitations. Symptoms occurring during an Adams-Stokes attack are suggestive of asystole duration: visual disturbances and dizziness occur after 3 to 5 seconds, loss of consciousness follows after 10 to 15 seconds, and seizures develop after 20 to 30 seconds. More severe symptoms are usually associated with advanced second-degree or third-degree AV block, particularly occurring in the distal conduction system.
DiagnosisTop
1. ECG, Holter monitoring or ECG recorders, and implantable recorders are used in patients with infrequent but severe symptoms. Patterns of abnormalities:
1) AV block: Figure 3.2-2.
2) Right bundle branch block and left bundle branch block: Figure 3.2-3.
2. Electrophysiologic study (EPS) is used in case of diagnostic uncertainties.
TreatmentTop
1. Management of symptomatic bradycardia: Figure 3.2-4.
2. Long-term management: Cardiac pacing is electrical cardiac stimulation. A pacemaker consists of a pulse generator and one or several leads. Pacing may be intermittent or continuous. Pacemakers have several programmable parameters such as heart rate, output (voltage and duration), and response to arrhythmias.
Pacemakers are marked with an international letter-coding system. Consecutive letters in the code denominate:
1) Chambers paced (A, atrium; V, ventricle; D, dual, both atrium and ventricle).
2) Chambers sensed (A, V, D, as above; O, absence of sensing).
3) Response to sensing (I, inhibited; T, triggered [an event triggers pacing from the device, ie, event A triggers pacing in the ventricle]; D, dual; O, no response).
4) Rate modulation, for instance, to exercise (O, none; R, rate response: pacing rate increases with activity).
5) Multisite pacing (A, atrium; V, ventricle; D, dual; O, no multisite pacing).
The most frequently used pacing modes:
1) VVI: Single chamber ventricular pacing (pacing inhibited by a sensed ventricular event).
2) AAI: Single chamber atrial pacing (pacing inhibited by a sensed atrial event; this mode is infrequent in clinical practice).
3) VDD: Ventricular pacing synchronized with atrial rhythm and inhibited by ventricular rhythm.
4) DDD: Dual-chamber pacing and sensing with inhibition and tracking (also known as synchronous pacing, aimed at maintaining AV synchrony).
New leadless devices enable ventricular stimulation and are useful to avoid lead-related problems.
Late complications of pacemaker implantation include lead dislodgement or damage affecting pacing or sensing/detection, pacemaker damage, pacemaker-induced tachycardia, increased pacing threshold, pacemaker syndrome (AV dissociation in patients with VVI pacemakers, which leads to reduced cardiac output and atrial contractions while AV valves are closed, consequently resulting in syncope, dizziness, fatigue, and neck pulsation), local infection, infective endocarditis related to a foreign body (cardiac device–related infective endocarditis), and very rarely sepsis.
FiguresTop
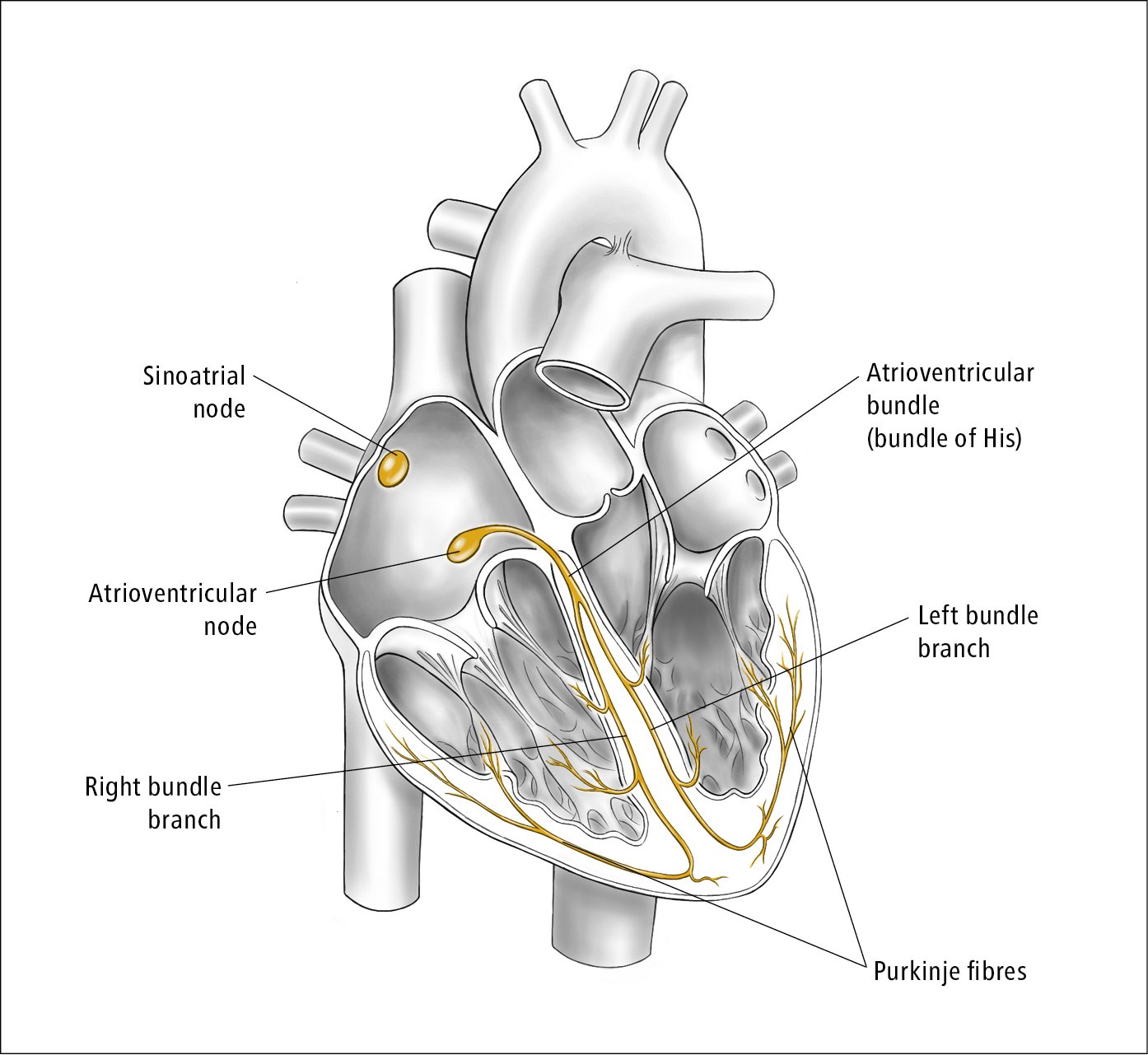
Figure 3.2-1. Cardiac conduction system. Illustration courtesy of Dr Shannon Zhang.
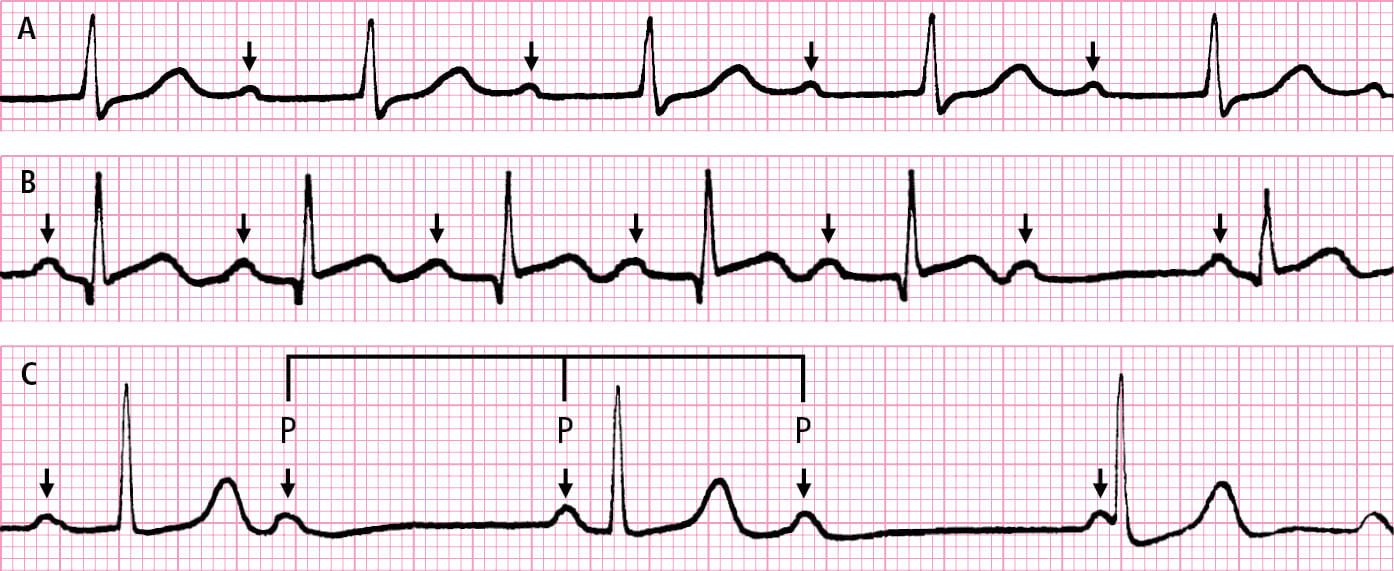
Figure 3.2-2. Atrioventricular (AV) block. A, prolonged PR interval (first-degree AV block). B, loss of the QRS complex preceded by progressive prolongation of the PR interval (Mobitz type I [Wenckebach] second-degree AV block). C, independent rhythm of P waves and QRS complexes (third-degree AV block, AV junction escape rhythm). The PP intervals separated by the QRS complex are shorter than the PP intervals not separated by the QRS complex (arrows indicate P waves).
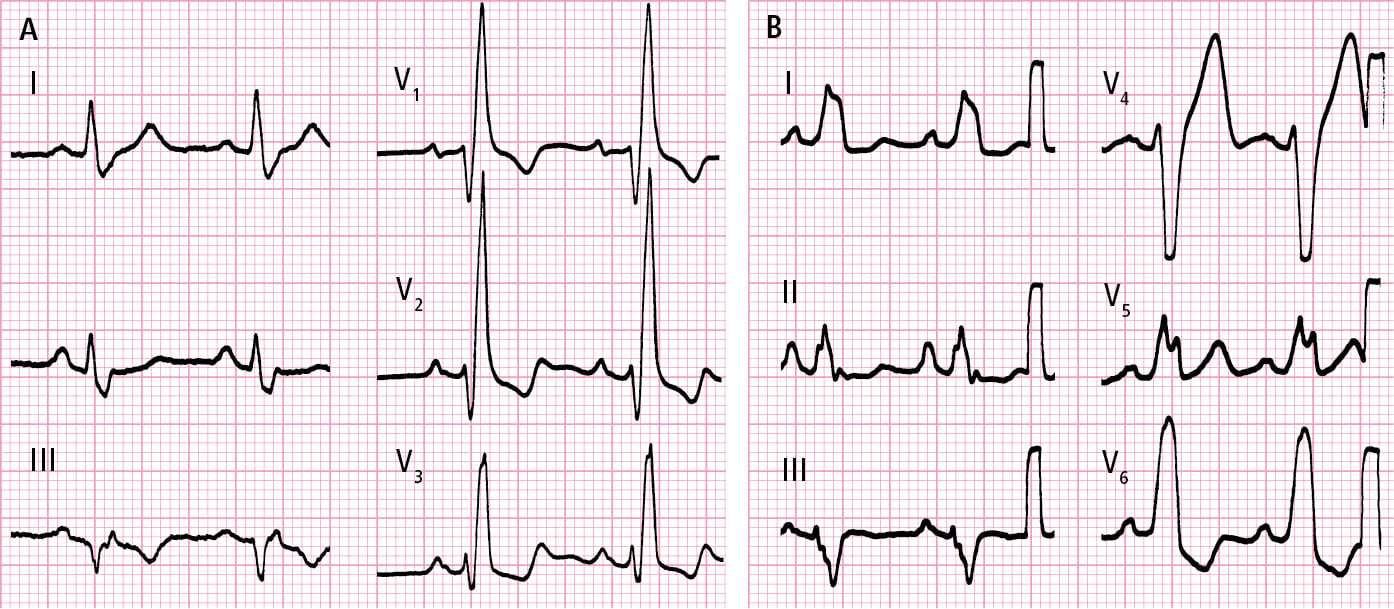
Figure 3.2-3. A, right bundle branch block. B, left bundle branch block.
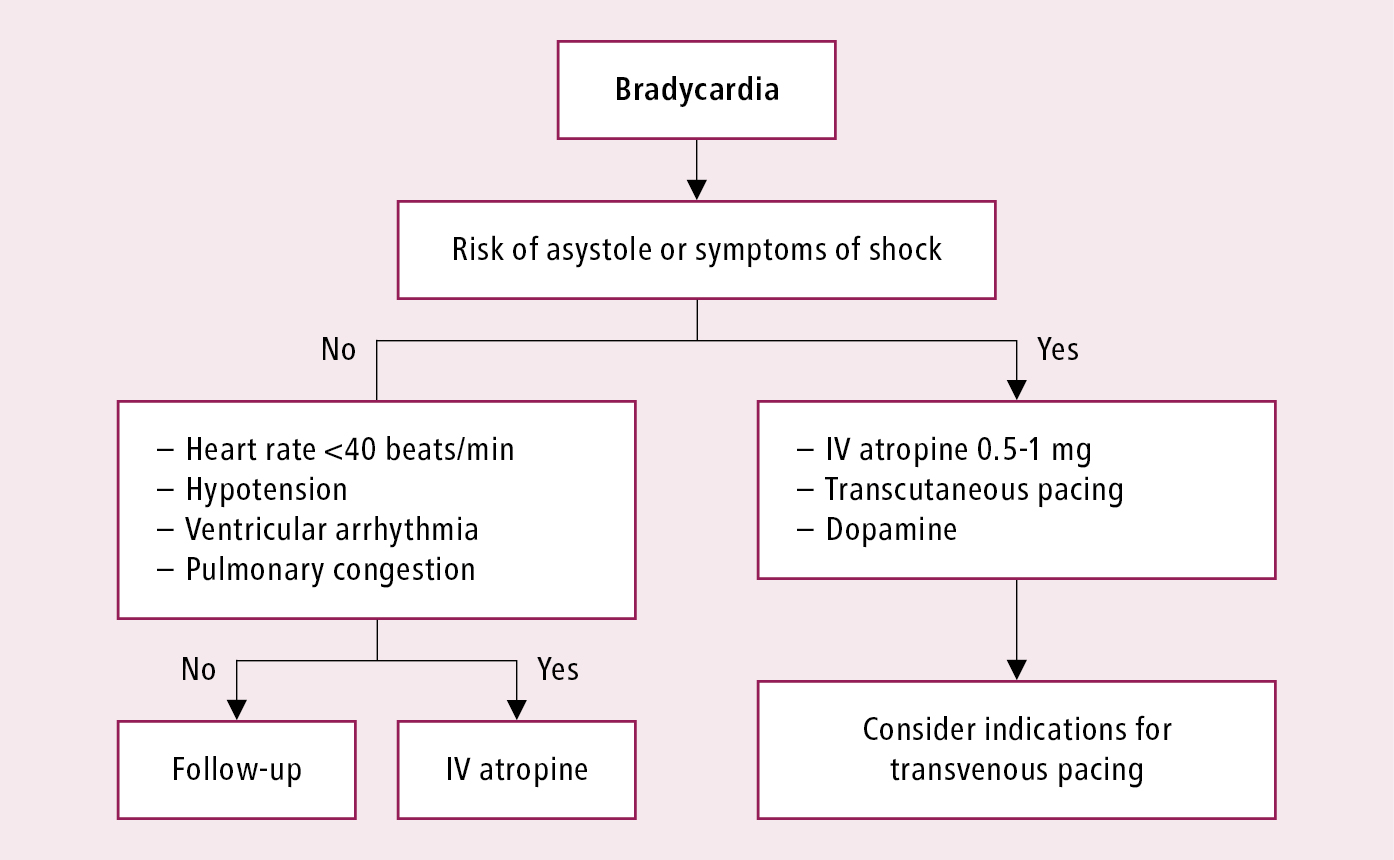
Figure 3.2-4. Management of bradycardia.