AASLD-IDSA HCV Guidance Panel. Hepatitis C Guidance 2018 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin Infect Dis. 2018 Oct 30;67(10):1477-1492. doi: 10.1093/cid/ciy585. PubMed PMID: 30215672.
European Association for the Study of the Liver. EASL Recommendations on Treatment of Hepatitis C 2018. J Hepatol. 2018 Aug;69(2):461-511. doi: 10.1016/j.jhep.2018.03.026. Epub 2018 Apr 9. PubMed PMID: 29650333.
Shah H, Bilodeau M, Burak KW, et al; Canadian Association for the Study of the Liver. The management of chronic hepatitis C: 2018 guideline update from the Canadian Association for the Study of the Liver. CMAJ. 2018 Jun 4;190(22):E677-E687. doi: 10.1503/cmaj.170453. PubMed PMID: 29866893; PubMed Central PMCID: PMC5988519.
Grgurevic I, Bozin T, Madir A. Hepatitis C is now curable, but what happens with cirrhosis and portal hypertension afterwards? Clin Exp Hepatol. 2017 Dec;3(4):181-186. doi: 10.5114/ceh.2017.71491. Epub 2017 Nov 16. Review. PubMed PMID: 29255805; PubMed Central PMCID: PMC5731432.
Guidelines for the Screening Care and Treatment of Persons with Chronic Hepatitis C Infection: Updated Version. Geneva: World Health Organization; 2016 Apr. PubMed PMID: 27227200.
Definition, Etiology, PathogenesisTop
Chronic hepatitis C is a chronic (>6 months) disease characterized by hepatic necroinflammatory changes caused by persistent hepatitis C virus (HCV) infection (see Acute Hepatitis C). The chronic infection results in inflammation, necrosis, and regeneration of hepatocytes that develop over time and may lead to the development of cirrhosis and, potentially, hepatocellular carcinoma (HCC).
Clinical Features and Natural HistoryTop
Clinical manifestations are similar to chronic hepatitis B. The majority of patients remain asymptomatic. Of those who are symptomatic, nearly 70% may report ≥1 of the following extrahepatic symptoms: fatigue, myalgia, arthralgia, paresthesia, pruritus, dry mucosae, secondary Raynaud phenomenon, or depressed mood.
In contrast to acute HCV infection, spontaneous HCV clearance rates in patients with chronic infection are extremely rare (~0.03% per year). The progression of the disease is slow and depends on the dynamics of liver fibrosis and cirrhosis. However, it is twice as rapid in patients with elevated alanine aminotransferase (ALT) levels (~40% of infected patients).
DiagnosisTop
Diagnostic algorithm: Figure 7.3-4.
1. Laboratory tests include complete blood count (CBC), liver enzymes (aspartate aminotransferase [AST], ALT, alkaline phosphatase [ALP]), other tests of liver function (bilirubin, international normalized ratio [INR], albumin), and creatinine levels. ALT levels are normal in ~30% of patients, and in some they are only periodically elevated (increases may follow a sinusoidal pattern). Thrombocytopenia, elevated bilirubin, or elevated INR suggests advanced fibrosis or cirrhosis.
2. Serologic and virologic tests include antibodies to HCV, HCV RNA, HCV genotype (this helps determine treatment type). Additional investigations should include testing for possible coinfections: hepatitis B surface antigen (HBsAg), anti-HBs antibody, anti-HBc antibody, HIV.
False-negative results of HCV antibodies may be seen over the first 4 to 10 weeks of infection or in immunocompromised patients, including those treated with hemodialysis (in this group consider measurements of HCV RNA as part of the initial diagnostic workup). In the acute phase there may be also periods of undetectable HCV RNA. If testing for HCV antibodies is positive and HCV RNA is negative, retest for HCV RNA (or HCV core antigen, if available) 12 and 24 weeks later to confirm the negative result.
To determine treatment, it is helpful to establish the viral genotype by a molecular method (polymerase chain reaction [PCR]) and, in the case of genotype 1, establish the subgenotype (GT1a or GT1b).
3. Noninvasive assessment of the extent of fibrosis:
1) Transient elastography (specialized ultrasonography measuring the degree of fibrosis).
2) Biochemical markers (AST to platelet ratio index [APRI], FIB-4 index; both available at mdcalc.com).
In all patients it is important to identify cirrhosis because of increased risk of HCC and decreased treatment response. The finding is also used to guide surveillance.
4. Liver biopsy with histologic examination of specimens: This may be indicated in case of suspected liver comorbidity, discrepancy between the results of noninvasive tests and the patient’s clinical status, or discrepancy between test results.
5. Clinical scores designed to measure the severity of liver disease, for example, the Model for End-Stage Liver Disease and Serum Sodium Concentration (MELDNa) score (available at mdcalc.com).
Positive HCV RNA in blood for >6 months from infection (the World Health Organization [WHO] definition). Biopsy is not required.
As in chronic hepatitis B.
TreatmentTop
Abstinence from alcohol (as alcohol increases liver injury and accelerates progression to cirrhosis) and smoking cessation is recommended. Hepatitis A or B vaccination in patients susceptible to infection with hepatitis A or B virus. In obese patients introduce a body-weight reduction plan. There are no contraindications to work (except for heavy physical work) or regular daily activities including sports, unless the presence of blood-borne infection precludes specific activities (eg, some medical exposure-prone procedures).
Guidelines from North American, European, and WHO expert panels may reflect local judgment and availability regarding treatment. Input from local experts may be helpful in some cases. Presented below are general considerations based on such guidelines. For specific treatments, please refer to the documents listed at the top or bottom of the screen under Additional Information.
Any patient infected with HCV should be considered for treatment.
1. Objective: Eradication of HCV, as this significantly reduces the risk of developing liver cirrhosis and HCC.
2. Key priority populations for treatment:
1) Patients with a new diagnosis or recurrence of hepatitis C.
2) Patients awaiting liver transplant:
a) MELDNa score <18-20: Start treatment before liver transplant.
b) MELDNa score ≥18-20: Liver transplant is performed without prior antiviral treatment and HCV infection is treated after the operation. If the waiting time for transplant is >6 months, start treatment before the operation.
3) Patients after liver transplant with reactivation of HCV infection.
4) Patients treated for chronic renal disease (including hemodialysis), especially those awaiting renal transplant.
5) Patients with HBV or HIV coinfection (or both).
6) Patients at risk of rapid liver dysfunction progression due to a coexisting liver disease or with extrahepatic manifestations of chronic hepatitis (see Complications, below).
7) Individuals at risk of transmitting HCV:
a) People who inject drugs.
b) Men who have sex with men (MSM) with high-risk sexual practices.
c) Women of childbearing age who wish to get pregnant (currently antiviral treatment of patients who are pregnant is not recommended).
d) Incarcerated individuals.
3. Treatment regimens depending on HCV genotype (based on the 2018 Canadian Association for the Study of the Liver [CASL] guidelines): A combination of direct-acting antiviral (DAA) agents is the current standard of therapy. It relies on combining nucleoside reverse transcriptase inhibitors (NRTIs), nonnucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors, entry and integrase inhibitors (a combination of 2-4 agents among nonstructural protein 3 [NS3], 5A [NS5A], and 5B [NS5B] inhibitors), and/or adding ribavirin. DAA monotherapy is unacceptable due to the risk of selection of resistant strains. In the past, treatment used to include interferon, but it has been mostly replaced by DAA therapy. The choice of regimen and duration of treatment are determined by:
1) HCV genotype.
2) Stage of liver fibrosis and presence of cirrhosis.
3) Previous treatment and its outcomes (no response, partial response, or relapse without a sustained virologic response).
4) Coexisting diseases (eg, renal failure) and the possibility of discontinuation of other drugs that have interactions with the planned treatment.
5) Local conditions (eg, the possibility of funding).
Available common regimens (see 2018 CASL guidelines for details [available from the website of the Canadian Medical Association Journal]):
1) Genotype-specific regimens:
a) Elbasvir/grazoprevir (genotypes 1 and 4).
b) Sofosbuvir/ledipasvir (genotypes 1, 4, 5, 6; genotype 3 requires ribavirin in conjunction).
c) Paritaprevir/ritonavir/ombitasvir/dasabuvir (genotypes 1 and 4; now rarely used).
d) Sofosbuvir/daclatasvir (genotypes 1, 2, and 3; daclatasvir is not available in Canada).
2) Pangenotypic regimens:
a) Glecaprevir/pibrentasvir.
b) Sofosbuvir/velpatasvir.
If previously treated with DAA agents, patients with or without cirrhosis can try sofosbuvir/velpatasvir/voxilaprevir. In European guidelines this combination is also recommended in treatment-naive and treatment-experienced patients with compensated cirrhosis.
Important contraindications:
1) Agents inducing cytochrome P450 and P-glycoprotein (carbamazepine, phenytoin) are contraindicated because of the risk of significantly decreased DAA concentrations and the resulting high risk of virologic failure.
2) Do not use NS3/4A protease inhibitors (grazoprevir, glecaprevir, paritaprevir, voxilaprevir, simeprevir) in patients with Child-Pugh B or C decompensated cirrhosis (see Table 7.3-3) or in those with previous episodes of decompensation, as higher concentrations of these agents result in increased risk of toxicity.
3) In patients with an estimated glomerular filtration rate (eGFR) <30 mL/min/1.73 m2, sofosbuvir should be used only if no alternative treatment is available.
4. Criteria of response to treatment:
1) Negative serum HCV RNA levels (<15 IU/mL) at 12 weeks or 24 weeks after the end of treatment.
2) Alternatively, negative serum HCV core antigen <3.0 fmol/L, if available, at 24 weeks after the end of treatment.
5. Potential drug interactions: Interaction checker from the University of Liverpool available at www.hep-druginteractions.org.
Follow-UpTop
DAA and ribavirin toxicity should be monitored. Liver enzymes and creatinine levels should be measured every 4 weeks and as clinically indicated. In patients with severe adverse reactions treatment should be discontinued (dose reduction is not used); this includes a >10-fold increase in ALT at any time; or a <10-fold increase in ALT with symptoms or significantly elevated bilirubin, ALP, or INR. If there is a <10-fold increase in ALT and the patient is asymptomatic, repeat testing should be performed every 2 weeks and therapy should be discontinued if the levels remain elevated. For regimens with ribavirin, it is also important to monitor hemoglobin, initially after 1 week and then every 4 weeks. In cases of severe hemolytic anemia (<2% of patients), treatment should be discontinued.
Annual HCV RNA testing is recommended in patients with ongoing exposure risks. Assessment of fibrosis should also be completed every 1 to 2 years. Patients with cirrhosis should be monitored for HCC every 6 months. If cirrhosis is identified, esophagogastroduodenoscopy should be completed to screen for esophageal varices.
ComplicationsTop
1. Cirrhosis: Without effective treatment, cirrhosis can develop in ~20% of patients with chronic HCV infection over a period of 20 to 50 years. Risk factors for accelerated progression to cirrhosis include alcohol, male sex, infection age >40 years, overweight or obesity, tobacco smoking, elevated serum iron levels, fatty liver disease, infection with HCV genotype 3, diabetes mellitus, HBV/HIV coinfection, and blood transfusion–related infection. Liver transplant may be indicated in patients with liver failure caused by cirrhosis.
2. Extrahepatic, autoimmune, and immune complex–related diseases:
1) Renal: Membranoproliferative or membranous glomerulonephritis (from asymptomatic hematuria and proteinuria to nephrotic syndrome and chronic kidney disease).
2) Dermatologic: Purpura (inflammation of small vessels of the skin), lichen planus, porphyria, psoriasis (especially in patients treated with interferon).
3) Hematologic: Immune thrombocytopenia, mixed cryoglobulinemia, lymphoma.
4) Neurologic: Peripheral neuropathy (usually sensory), cerebral vasculitis.
5) Rheumatologic: Arthritis (symmetric inflammation of numerous small joints similar to rheumatoid arthritis or inflammation of ≥1 large joint), Sjögren syndrome, antiphospholipid syndrome, systemic lupus erythematosus.
6) Cardiovascular: Vasculitis, arterial hypertension.
3. HCC: HCC may develop within 20 years in ~3% to 5% of patients with chronic hepatitis C. The risk is significantly increased (1%-2% per year) in patients with cirrhosis (HCC without liver fibrosis is rare) and decreased with successful antiviral treatment. Additional risk factors include age >60 years, increased ALP, and thrombocytopenia.
PrognosisTop
Sustained virologic response with DAA combination regimens is achieved in >90% of participants of clinical studies; in some subgroups the response rate may approach 100% of patients.
In patients with compensated cirrhosis the 5-year and 10-year risks of esophageal variceal bleeding are ~2.5% and 5%, respectively. The risk of decompensation of cirrhosis (ascites) in these patients is 7% and 20%, respectively, and the 10-year risk of encephalopathy is ~2.5%. Within 10 years, progression to end-stage liver failure occurs in 30% of patients with compensated cirrhosis. Mortality rates are 20% after 10 years in patients with compensated cirrhosis and 50% after 5 years in patients with symptomatic liver failure. In each case the prognosis is markedly improved after successful virus eradication, although cirrhosis and portal hypertension usually persist, particularly if other causes are still present (eg, alcohol use, nonalcoholic steatohepatitis).
PreventionTop
As in acute hepatitis C. Treatment of acute hepatitis C reduces the risk of developing chronic hepatitis C.
ScreeningTop
Screening is recommended in the following situations:
1) Risk factor–based screening:
a) History (present or past) of injection drug use.
b) Received blood transfusion, blood products, or organ transplant before 1992 in Canada.
c) History (present or past) of incarceration.
d) People who were born or lived in areas endemic for hepatitis C (prevalence >3%): Central/East/South Asia; Australasia and Oceania; Eastern Europe; sub-Saharan Africa; North Africa; Middle East.
e) Offspring of an HCV-infected mother.
f) History of sexual contact with HCV-positive individuals.
g) HIV positivity.
h) Chronic hemodialysis.
i) Elevated ALT.
2) Population-based screening: In Canada, individuals born between 1945 and 1975.
FiguresTop
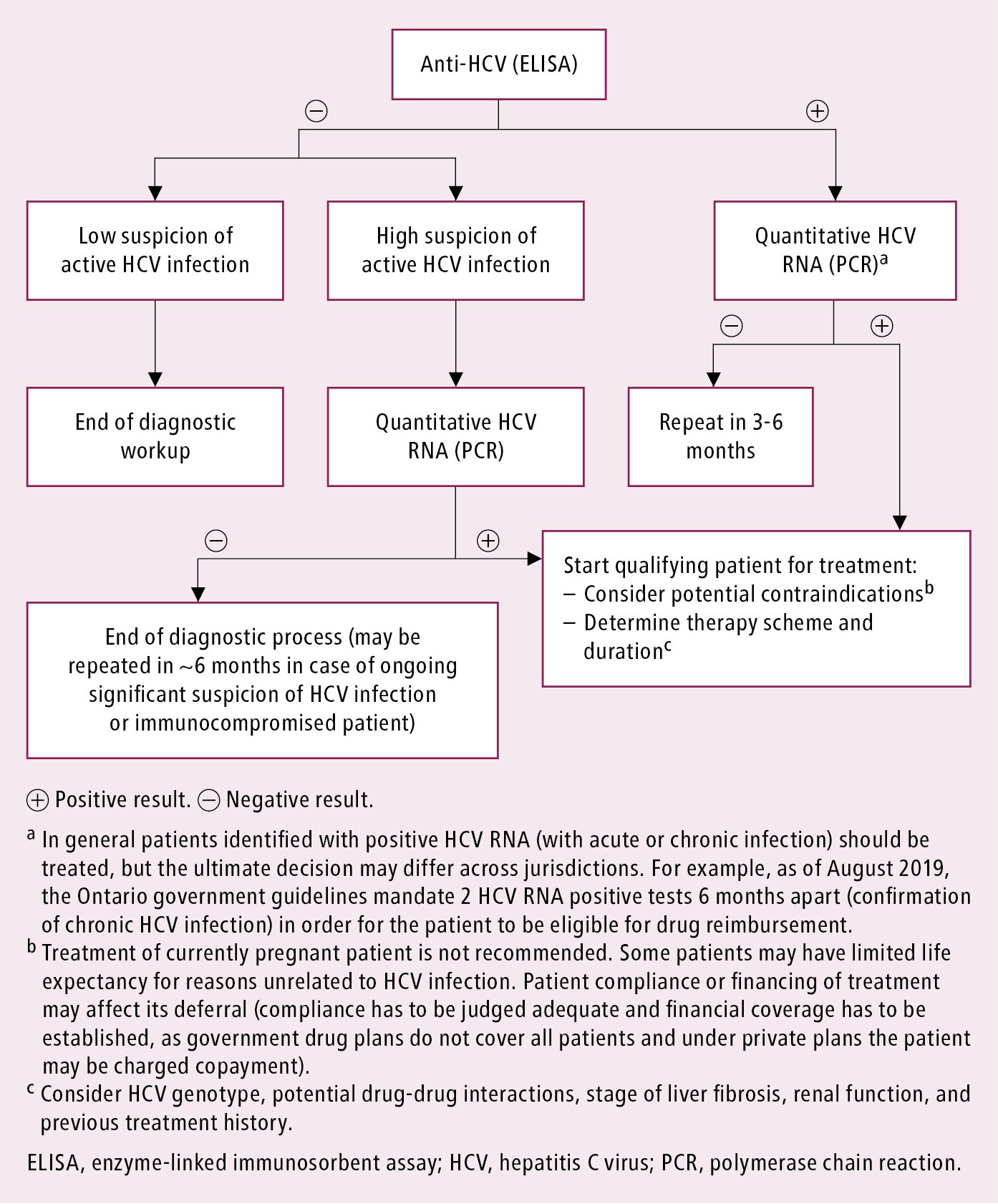
Figure 7.3-4. Diagnostic algorithm in patients with hepatitis C virus infection.