Asciak R, Bedawi EO, Bhatnagar R. British Thoracic Society Clinical Statement on pleural procedures. Thorax. 2023 Jul;78(Suppl 3):s43-s68. doi: 10.1136/thorax-2022-219371. PMID: 37433579.
Wolfe KS, Kress JP. Risk of Procedural Hemorrhage. Chest. 2016 Jul;150(1):237-46. doi: 10.1016/j.chest.2016.01.023. Epub 2016 Feb 2. PMID: 26836937; PMCID: PMC6026252.
Pleural drainage is performed to remove air, blood, or fluid from the pleural cavity; alleviate shortness of breath; achieve lung expansion; and correct mediastinal shift that may cause hemodynamic abnormalities. The procedure described below uses a chest drain. Emergency decompression of tension pneumothorax: see Pneumothorax. Decompression of pneumothorax using a syringe and catheter: see Pneumothorax. Thoracentesis: see Thoracentesis.
IndicationsTop
1. Pneumothorax:
1) Primary spontaneous pneumothorax persisting (>2 cm on chest radiography) after aspiration using a catheter and syringe. Note that a larger amount of aspirated air (>2.5 L) may indicate ongoing air leakage.
2) Secondary or iatrogenic spontaneous pneumothorax, excluding asymptomatic patients with a small (<2 cm) pneumothorax.
3) Tension pneumothorax.
4) Bilateral pneumothorax.
5) Hemorrhagic pneumothorax (hemopneumothorax).
6) Mechanical ventilation–induced pneumothorax.
7) Posttraumatic pneumothorax in patients with penetrating chest injuries.
2. Pleural effusion:
1) Malignant (drainage could be combined with pleurodesis: see Exudative Pleural Effusion Caused by Malignancy).
2) Complicated parapneumonic effusion or empyema.
3) Hemothorax.
4) Pleural effusion following surgery, including thoracotomy, esophageal resection, or cardiac surgery.
Potential ComplicationsTop
Subcutaneous emphysema; infection of the pleural cavity, skin, or intercostal tissues; incorrect tube positioning; lung injury; visceral injury; hemothorax; lung edema following expansion (re-expansion pulmonary edema); intercostal nerve injury; Horner syndrome (very rare).
Patient PreparationTop
1. Confirm the diagnosis of pneumothorax or pleural effusion using appropriate imaging. Studies include chest radiography (if pneumothorax or anatomy is doubtful, perform computed tomography [CT] of the chest) and ultrasonography of the pleural cavity. If time permits, prior to the procedure obtain a complete blood count (CBC) (including platelet count), international normalized ratio (INR), activated partial thromboplastin time (aPTT), and blood group and screen.
2. Obtain informed consent.
3. If the procedure is elective (which is rarely the case) and the patient is receiving anticoagulant treatment, discontinue vitamin K antagonists and wait for the INR to decrease to <1.5; discontinue direct oral anticoagulants (DOACs) 24 to 48 hours before the procedure, depending on the indication for anticoagulant therapy and thrombotic risk (see Perioperative Direct Oral Anticoagulant Management). For patients with mild laboratory coagulopathy (INR <3.0) who are not actively bleeding or receiving anticoagulants, we suggest no prophylactic plasma to correct coagulopathy for bedside chest drain insertion unless there are specific concerns around bleeding related to other patient characteristics (eg, antiplatelet drug use, drainage tube size, availability of ultrasonography or operator skill/experience).Evidence 1Weak recommendation against (harms likely outweigh benefits, but the balance is close or uncertain; an alternative course of action may be better for some patients). Low Quality of Evidence (very low confidence that we know true effects of the intervention). Quality of Evidence lowered due to the risk of bias and indirectness. Huber J, Stanworth SJ, Doree C, et al. Prophylactic plasma transfusion for patients without inherited bleeding disorders or anticoagulant use undergoing non-cardiac surgery or invasive procedures. Cochrane Database Syst Rev. 2019 Nov 28;11(11):CD012745. doi: 10.1002/14651858.CD012745.pub2. PMID: 31778223; PMCID: PMC6993082. The last prophylactic dose of low-molecular-weight heparin (LMWH) should be administered ≥12 hours before the procedure and the last therapeutic dose of LMWH should be administered ≥24 hours before the procedure.
4. Insert a peripheral venous catheter.
5. Place the patient lying on the side opposite the planned procedure with an upper limb elevated on the side of the procedure. In the event that an apical pneumothorax requires drainage, positioning the patient in the supine position with the bed head elevated to 45 degrees is appropriate.
EquipmentTop
1. Equipment for surgical field preparation (see Surgical Field Preparation for Small Procedures), infiltration anesthesia (see Infiltration Anesthesia), and medications for moderate sedation or short-term general anesthesia if necessary.
2. Chest drain and needle (bore 0.7-0.9 mm [22-20 gauge]) with syringe (10 or 20 mL). Small-bore chest drains are sometimes packaged in kits containing a needle and guidewire (as for central vein catheterization). In most situations including empyema chest tubes <14 French (F; 1F = 1 Charrière [Ch] = 1/3 mm), inserted using the Seldinger technique are preferred to large-bore chest tubes inserted using blunt dissection,Evidence 2Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to the observational nature of data and increased due to effect size. Chang SH, Kang YN, Chiu HY, Chiu YH. A Systematic Review and Meta-Analysis Comparing Pigtail Catheter and Chest Tube as the Initial Treatment for Pneumothorax. Chest. 2018 May;153(5):1201-1212. doi: 10.1016/j.chest.2018.01.048. Epub 2018 Feb 13. PMID: 29452099. as they are associated with a significantly lower risk of complications during insertion and shorter duration of drainage and hospital stay than large-bore chest tubes.
3. If the chest drain is to be inserted using surgical technique, equipment for skin incision and dissection of the intercostal space is necessary. This includes a scalpel, surgical and anatomical forceps, and blunt curved hemostat.
4. Suturing equipment: Needle holder, 1.0 needle with thread, silk suture.
5. Three-chamber chest suction unit (fill the suction pressure–regulating chamber [typically to a level of 10-20 cm] and the underwater valve chamber [to the mark] with a sterile fluid: Figure 21.13-1), connecting tubing, and low-pressure suction unit if required (a central [wall or bedside panel vacuum port] or electric suction device).
Site of Chest Drain InsertionTop
Always insert the chest drain at the superior margin of the rib.
1. Pneumothorax: The fifth to eighth intercostal spaces in the mid-axillary line or the second intercostal space in the mid-clavicular line.
2. Nonencapsulated pleural effusion: The fifth to eighth intercostal spaces in the midaxillary line.
3. Limited air or fluid collection: Depending on location determined using imaging studies and ultrasound guidance.
ProcedureTop
1. Chest drains used for pleural effusion should be inserted under imaging guidance. Use ultrasonography to guide chest tube insertion except in emergencies or when unavailable.
2. Prepare the surgical field (see Surgical Field Preparation for Small Procedures).
3. Perform local anesthesia (see Infiltration Anesthesia) and intercostal nerve block. Larger volumes are preferred over larger doses, therefore 1% lidocaine is preferred over 2%. IV conscious sedation is useful (see Procedural Sedation and Analgesia).
4. Puncture the pleural cavity using a syringe and needle (see Thoracentesis) to confirm the presence of air or fluid.
5. To insert a small-bore chest drain, use the Seldinger technique (pass the guidewire through the needle into the pleural cavity, withdraw the needle, dilate skin and intercostal soft tissue by a dilator, then remove the dilator, insert a chest drain over the guidewire, and finally remove the guidewire). The depth of chest tube insertion is dependent on chest wall thickness (measured by ultrasonography), ensuring that all side holes are inside the pleural cavity.
When using larger-bore tubes, make a ~1.5 to 2 cm skin incision at the level of the upper edge of the rib and dissect the intercostal tissue. Once the pleural cavity is entered (ie, the parietal pleura is penetrated), place a mattress stay suture. In patients with pneumothorax advance the chest drain towards the apex of the lung; in patients with pleural effusion advance the chest drain towards the base of the lung. The authors recommend against routine use of a chest tube with a trocar. If the chest drain is fitted with a trocar, withdraw the trocar ~1 cm within the tube before attempting chest drain insertion.
6. Connect the tube to the one-way valve suction unit (Figure 21.13-1). If active suction devices are used, the negative pressure should be from −10 to −20 cm H2O.
7. Secure the chest drain to the chest wall with suturing.
After the ProcedureTop
1. Check the position of the chest drain on chest radiography.
2. Monitor evacuated fluid volumes. Do not evacuate >1.5 L of fluid per hour. Monitor symptoms. If the patient develops repetitive coughing or chest pain, clamp the tube promptly. Check for evacuation of air from the pleural cavity (this is evidenced by air bubbles in the suction unit chamber [usually the middle chamber] fitted with an underwater seal valve). Make sure the suction system is airtight. Do not clamp the chest drain when air bubbles are seen inside or the drain is inserted for pneumothorax treatment, since pneumothorax can worsen if there is an active air leak.
3. Tube removal:
1) Indications: No fluid or airflow in the chest drain, complete lung expansion confirmed by chest radiographs (also after conversion from active to passive suction [eg, disconnection of the 3-chamber collection from suction]) for a period of several hours. The volume of fluid drained from the pleural cavity should be <200 mL/24 h.
2) Technique: We suggest topical lidocaine to reduce discomfort during removal for patients who have a chest tube.Evidence 3Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision. Watanabe SN, Imai K, Kimura T, et al. Effect of lidocaine cream analgesia for chest drain tube removal after video-assisted thoracoscopic surgery for lung cancer: a randomized clinical trial. Reg Anesth Pain Med. 2019 Nov 20:rapm-2019-100760. doi: 10.1136/rapm-2019-100760. Epub ahead of print. PMID: 31748424. Cut the securing suture. Instruct the patient to perform the Valsalva maneuver (ie, forced expiration with closed airway). Withdraw the chest drain at the time of the maneuver using a quick motion and immediately tie the stay suture to seal the tube track.
FiguresTop
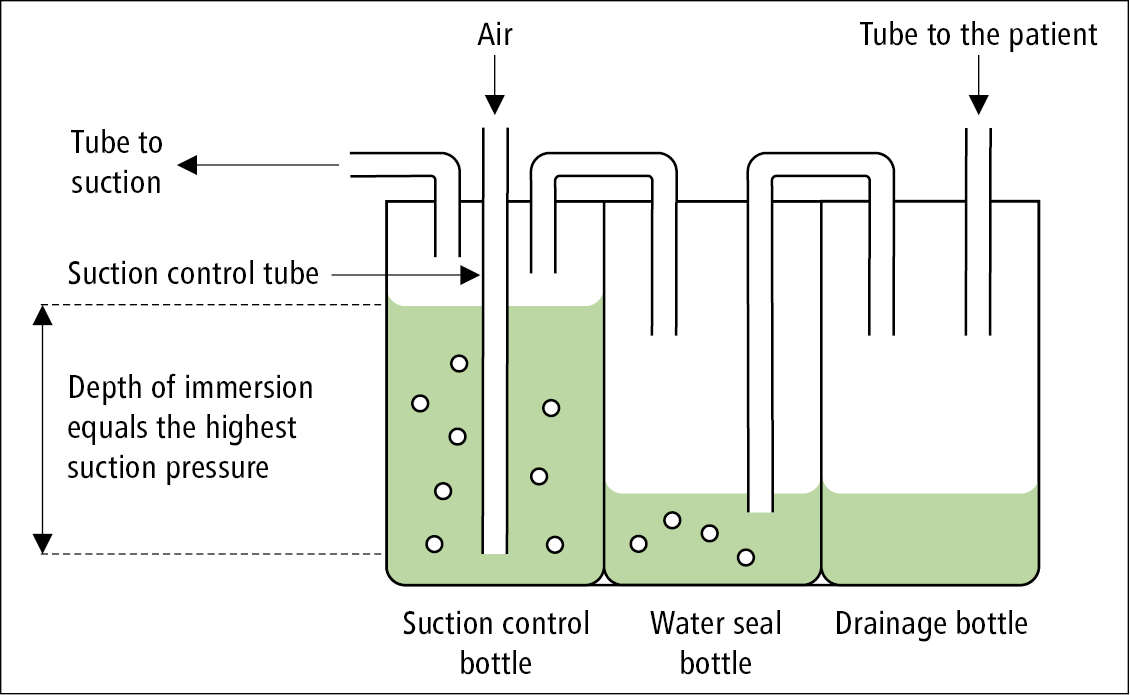
Figure 21.13-1. A 3-bottle chest drainage system.