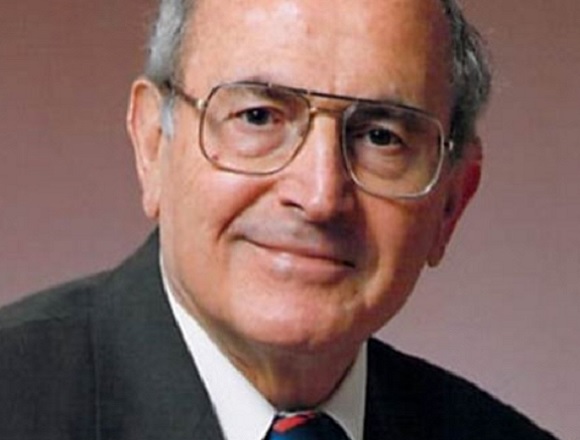
Dr Deepak L. Bhatt, director of Mount Sinai Heart, United States, researcher focused on interventional cardiology and cardiovascular disease prevention, and principal investigator in significant clinical trials, joins Dr Roman Jaeschke, critical care physician and methodologist, to reflect on the future of bariatric surgery, management of critically ill patients with high troponin levels, need for catheterization in non-ST-segment elevation myocardial infarction (NSTEMI), and management of chronic coronary artery disease (CAD) and lipid disorders.
Contents
- How to achieve academic success?
- A cardiologist in the world of bariatric surgery
- Troponins in critically ill patients
- When to send patients with NSTEMI to the cath lab?
- Chronic CAD: P2Y12 inhibitors vs ASA, colchicine
- Lipid management: triglycerides, LDL cholesterol
Transcript
Roman Jaeschke, MD, MSc: Good afternoon. Welcome to another edition of McMaster Perspective. This is a series where we interview leaders in different areas of medicine—here, cardiovascular medicine.
It’s my immense pleasure to introduce our guest today, Professor Deepak Bhatt, who has recently moved from Harvard Medical School to New York. I do not want to destroy his affiliations and title, so, Professor Bhatt, maybe you could tell us where you work? What’s your position at the moment?
Deepak L. Bhatt, MD, MPH: Yes, absolutely. First of all, thank you for having me. I am the director of Mount Sinai Heart in New York City, where I’m the Dr Valentin Fuster Professor of Cardiovascular Medicine.
Roman Jaeschke: Thank you very much. Professor Bhatt, maybe the first question. When preparing myself for this interview, I’ve seen several hundreds of publications. I think there were several in June alone. How come you are so prolific? What’s the advice to younger people or less prolific people to achieve this kind of success?
Deepak L. Bhatt: I don’t know that I’m a great source for such advice because the advice I follow is what my chair of medicine gave me when I was first negotiating for a job at Cleveland Clinic. I asked Dr Jim Young, a famed heart failure doctor, where my protected research time was, and he said, “Oh, don’t worry about that. You’ve got tons of it on nights and weekends.” You know, of course, he was saying that tongue in cheek, and probably younger people these days don’t find it even funny. They, I think, properly think about things like work-life balance much more now than a few decades ago. But in fact, I did take his advice to heart and really at that point itself got in the habit of doing a lot of research on nights and weekends once the clinical work was done. For better or worse, I’ve kept that pattern up through the life.
But that’s why I hesitate to share that with you and your audience, because I don’t know that is something that I would necessarily endorse as a way to balance life in a healthy manner. But for folks that really do want to be very academically productive, there’s really no shortcut other than putting in lots of time and effort.
Of course, sometimes it can be useful to structure one’s job so that there is actual protected research time that isn’t nights and weekends, but it’s actually during the regular workweek. I was quite successful at doing that for part of my time, say, when I was just in Boston at the Mass General Brigham health-care system at Harvard Medical School, where you have funding for doing research—then you can usually carve out time that’s dedicated to doing research.
I guess for people who are really interested in doing research, and writing, and trying to be prolific, it does help to have protected research time, but you’re not going to have that in general in most places unless there’s some source of funding for that, whether it’s governmental funding, industry funding, philanthropic funding. I guess that would be my answer to your question.
Roman Jaeschke: This story that you mentioned is quite funny. I suspect that I will start using it from now on. I also suspect that even if you had complete 40-hour protected time, you will be nowhere near productivity. It’s simply not enough time. However, we call that time protected.
Deepak L. Bhatt: I also try to multitask. I mean, sometimes people are in a train, or a taxi, or an Uber, or something, and some people daydream, some chat. I typically try to get work done. Same thing if I’m on a flight. I find those times actually really useful to get things done. If I’m sitting around in the airport, some people get really anxious, or angry, or just feel like it’s a waste of time, but I feel like those moments are actually protected time in a manner of speaking to get academic work that I like done. I think that can be useful.
Other things that help it… I mean, it’s really useful to have great collaborators and, for example, to work with great fellows who many times will serve as the first author on a paper and will write the first draft. If it’s a talented fellow, typically it’s in a very good shape. Likewise, working with other coauthors around the world who themselves are good data analysts, and physician scientists, and writers certainly helps the collective productivity. I mean, you’re at a place with best university. There are a lot of prolific people there, or as a matter of fact, in a variety of areas of medicine. I’ve had the good fortune to collaborate with a number of them and actually learn a lot from them as well, including about how to write efficiently, effectively, quickly.
Roman Jaeschke: That’s, I think, a very useful conversation for a lot of younger people, aspiring… including the need to concentrate, need to be in the proper environment, need to have collaborators, need to work with junior people and spend enough time and energy on it. Thank you very much for all this.
Now, looking through your publications, I was, again, almost surprised by the breadth of your interest. Where would you say your biggest contribution and achievements in the cardiovascular field lie?
Deepak L. Bhatt: Thanks for that question. You’re right. I have always had a really diverse set of interests. That’s just been true my whole life and I’m happy with that, but perhaps a word of caution, especially to some of the younger folks who are starting off in their careers right now about that. There’s something to be said about having a lot of interests. I mean, the general advice in academic life is to have an area of focus and area of clear expertise. Certainly that was always the advice at Harvard Medical School if one wanted to climb the academic ladder, that you were going to be much more likely to be successful, make it to full professor, if it was clear that you are an international expert in something, even if it were a relatively narrow area, versus being pretty an expert in a whole bunch of areas. I think that’s true at many or perhaps most universities.
I think there is a little risk of saying, “Oh, I’m interested in this this month, then I’m going to do this type of research and writing, and 6 months from now I’m going to do something else.” I don’t know that I would, generally speaking, recommend that approach. I think the overarching principle should always be do what you find interesting, because if you don’t find something intellectually interesting and if it doesn’t really get your juices flowing, then you shouldn’t be doing it because it’s a waste of your time, and your life, and it probably won’t be that professionally successful anyway. I think it’s really important to be passionate about what you’re doing.
For myself, I’ve just had a variety of interests and I pursue them. Some of those things pan out, some haven’t, but that’s okay. That’s science, including science as it pertains to clinical medicine. I’ve been really lucky to work with great folks and to also work with folks from different backgrounds. I just never thought, “Oh, I’m a cardiologist, therefore I will only work with cardiologists.” In fact, I think some of the best collaborations are when people go out of their own narrow disciplines, work with folks from other areas of human endeavor, and really come up with things that are unique.
I mean, one example and something I’m proud of is the STAMPEDE trial. It is an acronym I came up with for a trial that actually was the first randomized clinical trial of bariatric surgery, sometimes now called metabolic surgery. There have been a lot of great data showing that bariatric surgery caused large degrees of weight loss. We didn’t need a randomized clinical trial to show that, that’s obvious, but what hadn’t really been done was an examination to see how bariatric surgery performs with respect to diabetes and, in particular, resolution of diabetes. That’s what led to the STAMPEDE trial.
It was designed when I was at Cleveland Clinic. I was really proud to play an instrumental role in its design and I was one of the coinvestigators, who were myself, and an endocrinologist, Dr Kashyap, and a bariatric surgeon, Dr Schauer. And the three of us really did something that I thought was quite valuable to the field. We brought randomization to bariatric surgery and showed a very significant difference versus just best medical therapy in terms of things like resolution of diabetes. Subsequently other trials have confirmed it.
That was work published in the New England Journal of Medicine and I think it was 2012, and 2014, and then the 5-year follow-up in 2017. That’s something where you might think, “How did a cardiologist get into that?” But that’s because I was always interested in clinical trial design and doing things that were novel, and bringing rigorous methodology to areas of medicine and surgery and related fields. It hadn’t happened before.
Roman Jaeschke: Maybe I will follow it because I just found that you influenced my life because I spent a good few years in a bariatric clinic preparing people to bariatric surgery and then seeing them after surgery and seeing an absolutely immense positive impact on quality of life, which those people experienced.
My question is maybe outside your area of current research interest, but how do you see bariatric surgery at the time of availability of new drugs, of which we keep hearing: glucagon-like peptide-1 (GLP-1) receptor agonists, then glucagon influencing… Will the role of bariatric surgery persist or will it be replaced somehow by medications?
Deepak L. Bhatt: This is a terrific question. I’m interested in obesity in terms of lifestyle and dietary modification, I’m interested in terms of a metabolic surgery, as you and I just discussed, but I’m also interested in the medical therapy side of it as well. I find it all interesting.
In fact, I was a principal investigator (PI) of the first of the really large cardiovascular outcome trials of an obesity drug that did turn out to be such a happy ending. It was for rimonabant. There were some concerns about whether it increased depression and suicidality. Actually in our trial it didn’t increase suicidality, but there were concerns by regulatory agencies and we ended up having to stop the trial, probably a mistake on the part of the regulatory agencies.
But at any rate, I’ve been interested in all aspects of it. And I think that the drugs that are coming out now are really incredible in terms of the degree of weight loss that they provide. Many of these drugs are ones that were initially thought of as diabetes drugs but in fact produce pretty significant degrees of weight loss—the GLP-1 agonists. At least some of them have been shown to reduce cardiovascular outcomes, but they also cause a useful degree of weight loss.
Now there are even other sorts of more advanced agents along those axes. Tirzepatide, for example, is one where there’ve been some recent data showing the degrees of weight loss it produces. There are agents coming out… incretins, and agents targeting 3 different pathways. The degrees of weight loss seem to be correspondingly [greater with] the increasing number of pathways that are targeted and in some cases rivaling what bariatric surgery can produce.
I think the approach to obesity will likely be what in cardiology we do with coronary artery disease (CAD). Basically, we tell everybody: watch your diet, eat right if you can follow a plant-based diet, exercise, try to lose weight if you’re overweight, restrict calories to the extent that you can to prevent weight gain. But then, beyond that lifestyle modification, we also endorse the use of medical therapy, typically polypharmacy, addressing both cardiovascular risk, things like high cholesterol, but if people have symptoms—medicines like beta-blockers to address symptoms, and then for people where that doesn’t do the trick, we refer them on to procedures like stents or bypass surgery. I think it will be a similar paradigm in fact.
In the trial of the American College of Cardiology, I was a coauthor on a sort of review/opinion piece where we a few years ago really put that paradigm forth. That is lifestyle modification, of course, for everybody, medical therapy for those where that’s not sufficient, and where that doesn’t do the trick, go ahead with metabolic surgery. Even there, there’s a variety of different options from minimally invasive endoscopic approaches, reversible approaches, to a classic Roux-en-Y.
There are various degrees of invasiveness depending on patient preference, patient comorbidities, degree of weight loss that’s desired. I see these all as complementary approaches, so I don’t think any one thing will totally replace another. But I do think that the medicines that are out there right now and that are being evaluated and in some cases approved are going to have an enormous impact on obesity. Of course, right now, they can be depending on the health-care system, a little pricey, but eventually that problem will solve itself.
Roman Jaeschke: We ended up talking about something I didn’t expect, which is obesity. Let’s go to a few things that I’m interested in, which would be mostly in terms of CAD and maybe acute CAD.
I will abuse my position a little bit. I’m an intensivist. I work in the intensive care unit. When we have been looking at our patients recently, one of my dilemmas is what to do with elevated troponins, what to do with elevated cardiac enzymes. It’s not only postsurgical, but I would say equally frequently, if not more frequently, in septic people, in people with profound respiratory failure or in shock. I will ask you for a personal elevator-type advice for how to deal with those people. There are so many of them, it’s 40% to 50%.
Deepak L. Bhatt: It’s a great question. The thing with troponin is if you look, you often find, and the real question is, should you look?
I think troponins are most valuable when there is a suspicion of an acute coronary syndrome (ACS). If somebody comes into the emergency department clutching their chest, saying that they’re having chest discomfort, it’s valuable to get a troponin there because if it’s elevated, it probably is an ACS.
In that sort of situation, there is a lot of data supporting an early invasive approach or, in other words, going to the catheterization lab and often getting a stent, sometimes getting bypass surgery, sometimes getting medicines alone. For a real ACS, troponin positive, higher intermediate risk, with no contraindications, that’s what the data and the majority of guidelines support. So there things are pretty clear.
On the other hand, troponins can be elevated even in stable outpatients. In fact we saw this in the BARI 2D trial, in an analysis where Brendan Everett was the first author—he’s a cardiologist at Brigham—and I was the senior author. We published this in the New England Journal of Medicine a few years ago. We took patients from BARI 2D—and that was a trial of stable patients with diabetes; outpatients with multivessel CAD—and for the purposes of this analysis, there were 2 randomizations. That doesn’t matter. What we looked at was the baseline troponin levels and we found like a third of the patients in this stable outpatient population had elevated troponins to the point where if they just walked into an emergency department and instead of being a stable patient in a trial, were clutching their chest and said, “I’m having excruciating chest pain, there’s an elephant sitting on my chest,” we would have said, “Oh, well, this is an ACS.”
The point there was in high-risk but stable outpatient diabetes patients with multivessel CAD. There are a lot of positive troponins there. So you can imagine that if you actually have sick inpatients, even if they’re not there with an ACS, there’s going to be a lot of positive troponin, if those patients walking around in BARI 2D had a high prevalence of positive troponin using a highly sensitive troponin assay. The clinical context really matters.
Now, those patients that I mentioned, at BARI 2D, that were stable, not having an ACS but having a positive troponin, they were surely at a higher risk than the ones that didn’t have a positive troponin. It’s not that the positive troponin was, “Oh, that’s nothing, nothing to worry about.” No, it was something, I guess, to worry about if you measured it because they were at higher risk than the ones without troponin. You couldn’t explain it all the way with other sorts of measurable risk factors. So yes, if somebody is having troponin elevation versus someone that isn’t, even if they’re otherwise totally identical in terms of their diabetes status, cholesterol status, etc, they are still at a higher risk. Whether that’s a modifiable risk and actionable risk is debatable. In the context of ACS, it definitely is, because like I said, those patients, for example, could go to the catheterization lab.
And someone with sepsis, like you’re seeing in the unit… The positive troponin does tell you they’re going to do worse than the patient that doesn’t have a positive troponin. But again, unless there was a clinical reason to check it like suspected ischemia because of electrocardiographic (ECG) changes or a new wall motion abnormality on an echo, or they were suddenly hypotensive—more hypotensive than they were from the sepsis—there was some clinical reason that might make you do it. I’m not sure that other than for prognostic purposes or research purposes, it actually tells you how much that’s actionable other than maybe you’re going to be more worried about them, whether you should send that patient to the cath lab on that basis. I wouldn’t because they’re septic and they’ve got other things going on that you would need to be focusing on.
So sometimes troponins in a context other than what they were really designed for can provide useful prognostic information as long as physicians don’t act on that information inappropriately, like sending people with gastrointestinal (GI) bleeds or sepsis to the cath lab for a positive troponin unless there is in fact superimposed ACS.
Roman Jaeschke: I find that very instructive and useful, even including the fact that there is no black or white answer here. There is a continuum that will depend on the context and degree of elevation, presence of ECG changes, degree of suspicion, and the context of clinical intervention. You obviously would do it differently in somebody who is bleeding to start with or somebody who is for completely normal hemostasis and you will not be scared of interacting with it.
Deepak L. Bhatt: Absolutely. The echocardiogram can be your friend here. For sure the electrocardiogram can be useful. If that’s showing dynamic ST-segment depression [or] if it’s showing ST-elevation—well, obviously that’s a real ACS and something to worry about most of the time. On the other hand, if you do an echocardiogram and you don’t see any wall motion abnormality, it’s a good quality study, that’s reassuring. Someone with normal left ventricular function, no wall motion abnormality, even if the troponins are positive, their prognosis will probably be pretty good. Especially if they are there with some other diagnosis, then for sure, focus on that.
Roman Jaeschke: A follow-up question then. Say that this person survived sepsis, was in the hospital with nonspecific ECG changes, maybe a few-fold elevation on troponins, and a month later is at home follow-up. How far would you go trying to determine the degree of CAD?
Deepak L. Bhatt: It depends. I would, at a minimum, say perhaps this person has undiagnosed CAD. They just got out of hospital, they survived sepsis, they should be thankful for that. But let me look carefully now, that they’re an outpatient and have recovered, at their cardiovascular risk factors. Let me make sure: is the low-density lipoprotein (LDL) beyond what the guidelines recommend? What about their blood pressure? Should those be treated not just with lifestyle modification, but medical therapy?
So I would be more aggressive about identifying the risk factors and treating them, including with medical therapy, than I otherwise would. Would I go any further in terms of stress testing? It depends. If they were having symptoms, potentially, of cardiovascular disease, then I might go that next step and get a stress test if I thought maybe they were having angina. On the other hand, if they’re fully recovered from their sepsis, they’re biking to work every day, having no cardiovascular symptoms, there the guidelines wouldn’t recommend just doing testing for the sake of doing it. There I would probably just say, “Okay, I’ve checked you for risk factors. I’m treating them. You feel great. There’s nothing I can do to make you feel better since you feel great in terms of procedures. So other than modifying your cardiovascular risk factors with medical therapy, it’s better to leave you alone.”
Roman Jaeschke: All right. It is, again, useful. Maybe one other question about ACS. I’m operating in a hospital that does not have a cath lab. In order to get an angiogram, we have to send people outside and it’s cumbersome sometimes, and inconvenient, and whatnot. In terms of non–ST-segment elevation myocardial infarction (NSTEMI), what would be your criterion to say, “Okay, if you don’t have it, you should send the person to the cath lab now.” Could you give us some of your perspective of your own practice?
Deepak L. Bhatt: Absolutely. If someone has a true NSTEMI, that is, they’ve come in, the clinical presentation is correct, they’ve got some sort of ischemic syndrome, chest discomfort, or associated symptoms. So it sounds like it’s the real thing. Troponin has been measured, it’s clearly elevated. That patient has an NSTEMI and in general, unless there are contraindications, you should get a cardiac catheterization depending on just how high risks there are in the next 24 to 48 hours. I think that really is the standard of care in most urban centers around the world.
If there are ECG changes that are dynamic, of course, if there’s an ST-segment elevation, that’s an absolute emergency, you should go to the cath lab if it’s available. If one’s not available in a couple of hours, we probably should give them lytics and then still transfer them to a cath lab. But in the case of an NSTEMI, I think that it really depends on just at how high risk the patient is. If they’ve got dynamic ST-segment depression, they really should go to the catheterization lab pretty soon.
Some proportion of those patients are really a ST-segment elevation myocardial infarction (STEMI), where it’s something like the left circumflex or a large major diagonal of the left anterior descending artery that’s occluded—it just doesn’t show up on a 12-lead ECG as ST elevation, but they basically have ST elevation. Marked dynamic ST-segment depression—that should be treated almost like a STEMI and should go to the cath lab quickly. If the hospital doesn’t have one, transfer for one.
Other forms than STEMI, where the ECG doesn’t show any clear-cut dynamic ST-segment depression or ST-segment elevation, or anything like really hyperacute T waves, or something like that, there is basically a troponin elevation and an ECG that’s “normal,” there I think if the person is otherwise healthy, doesn’t have the sort of contraindications or comorbidities that perhaps should keep them out of a catheterization lab, those sorts of patients, I think, within 24 to 48 hours should get a catheterization done in part to identify their coronary anatomy and identify those patients who maybe don’t have severe CAD. It’s useful as a diagnostic test, but also then to identify those that do have severe stenosis where they do, I believe, benefit from revascularization—percutaneously, if it can be done safely, or surgically, if not. I think the bulk of data support that.
However, for low-risk patients where it’s a troponin that’s positive, but maybe it’s low-level positive, the story wasn’t really that good, there isn’t a catheterization lab nearby, they’ve stopped having chest pain on medical therapy, it’s not crazy or inappropriate or guideline discordant to do some evaluation noninvasively on that patient. In the 2021 American College of Cardiology/American Heart Association (ACC/AHA) guidelines, of which I was thankful to be a coauthor, there we gave 2 basic options. One is delineate the coronary anatomy noninvasively with a coronary computed tomography (CT) angiogram or do a conventional stress test. Regardless of which pathway you pick, depending on local hospital expertise, if that’s abnormal, then you probably really should go to the catheterization lab.
Roman Jaeschke: When you say “conventional,” you mean the regular stress test or with some imaging?
Deepak L. Bhatt: That’s a really great question. That will really vary depending on hospitals and expertise. My preference is to do an exercise stress test if possible, as opposed to a pharmacological stress test, because there’s a lot of other information.
For example, if some older person goes 10 to 12 metabolic equivalents (METs), it’s unlikely we’re going to do anything that’s going to make them do better or live longer. I mean, that’s pretty good. A procedure is probably not going to help them live longer. On the other hand, if they go 2 minutes and there are dynamic ST changes; ST-segment elevation, they get hypertensive; there’s other information from the stress test; and the electrocardiogram, and the blood pressure, and just even the heart rate response, the rhythm response—that can provide a lot of clues. That person, they’re not going to do well at home. There you really want to get them to the catheterization lab prior to hospital discharge.
So it depends. Personally—and this depends a bit on physician preference, on what’s available at the hospital—I like an exercise echocardiogram because it does provide to me some additional information in this patient that’s come in with some chest pain syndrome. It lets me evaluate their valves for any pericardial disease. Then the exercise portion does evaluate whether there’s a new wall motion abnormality with exercise. If there is, that’s a very specific way of saying, yeah, this actually probably is true, true and related, and we probably ought to get this patient to a catheterization lab.
Roman Jaeschke: I’m fascinated by this discussion. I just want to say that we used all the time I asked you for and I still have questions. Are you willing to continue for a little longer?
Deepak L. Bhatt: Sure.
Roman Jaeschke: That’s very kind of you. Let’s go for a second to chronic CAD. Two papers caught my eye when I looked at your most recent publication. One was the comparison of P2Y antiplatelet therapy with aspirin in, I believe, secondary prevention.
I’m curious on a short-term level, if somebody, in a social situation, were to tell you, “I have this disease, what should I be taking?”, do you have a preference and how much difference it may make?
Deepak L. Bhatt: A great question. There are now a number of trials to show that a P2Y12 inhibitor, at least in high-risk secondary prevention, is superior to aspirin. In fact, McMaster University many years ago contributed quite a bit to this data set. I don’t know if you recall, but there was an older trial called CAPRIE (it’s what initially led to the approval of clopidogrel), so clopidogrel alone versus aspirin alone, that showed that clopidogrel was more efficacious with less hospitalization for GI bleeding. So 75 mg of clopidogrel—we use lower aspirin doses now, but what at the time was 325 mg of aspirin—was both more efficacious and safer.
Now, was the degree of efficacy enormous versus aspirin? It was a modest benefit. Was the reduction in bleeding substantial? It was statistically significant, again, in magnitude modest, but still, for what’s now a generic drug—though even as a generic a bit more expensive than aspirin, which is extremely inexpensive. But for high-risk secondary prevention, why not? I think that the data now for P2Y12 inhibitor monotherapy—and now there’s also data for ticagrelor, not just for clopidogrel in specific situations—is pretty good. So for the right patient, yes, I think that is a good option.
Roman Jaeschke: Okay. So the bottom line for a person like me, in a system in which I can afford it, that would be a slightly preferred option.
Deepak L. Bhatt: For high-risk secondary prevention, yes, I think so. I mean, I believe that was true on the basis of CAPRIE many years ago. I mean, that was published in The Lancet back in 1993 or so, if I remember right. But more recently, there was a study from East Asia called HOST-EXAM, also published in The Lancet, that essentially corroborated what was seen in CAPRIE. It took high-risk stented patients, they got dual antiplatelet therapy, as the guidelines recommend, for a period of time, and when that was stopped, they were randomized to aspirin or to a P2Y12 inhibitor, and again, the P2Y12 inhibitor won.
Roman Jaeschke: Okay. The second question on secondary prevention. Do you use colchicine in your own practice? I have seen your name on the papers that examined that.
Deepak L. Bhatt: A terrific question. I haven’t done that to date, but that’s because it wasn’t an option in the United States to date. But just in the past, a month or so, the FDA did approve a particular formulation of colchicine for use in secondary prevention. So now it’s an option.
I think that the data so far are provocative. I think one should always keep an open mind about such things. I do believe that inflammation is extremely important in cardiovascular disease. My good friend Peter Libby at Brigham and Women’s [Hospital] and Harvard Medical School spent a lot of pioneering work in that area. And Paul Whittaker, also a good friend from those same institutions, has led trials that have shown that anti-inflammatory drugs, in fact, do reduce cardiovascular events. Canakinumab in particular is what I’m talking about.
So that anti-inflammatory hypothesis has been proven. Whether colchicine is a way to deliver it, there are strongly some provocative trials, but I just won’t opine further because I’m sure [this will be done by] the Data and Safety Monitoring Board of the largest ongoing trial of colchicine in cardiovascular disease that my good friends at McMaster University are running. I am waiting to see what that trial shows before I make an opinion about what’s happening.
Roman Jaeschke: Something to pay attention to. Professor Bhatt, the real question why I wanted to talk to you was metabolic [issues]—lipids and, specifically, triglycerides, if you are prepared to give us your perspective on that.
As I said, I’m an internist and critical care physician. I see a lot of people who come on statins. Some of them are on ezetimibe. We measure cholesterol, we sometimes measure triglycerides, and we nod our heads, yeah, it’s elevated, but I rarely see medications being used for it.
You are one of the pioneers in this area. Please give us your perspective of what should we be doing, what should we take into account, how should we behave, and why is the uptake not as wide as one would expect on the basis of publications?
Deepak L. Bhatt: Yeah, a great question. First of all, let me say for LDL cholesterol, the jury is in. Hopefully there aren’t still people out there... Well, I know there are others that are just denying the association between LDL cholesterol elevation and CAD, I mean, atherosclerosis in general. There’s no question they are linked and lower LDL is better.
If one has good genes and you’re lucky, the Mendelian randomization works quite clear that lower LDL lifelong due to good genes is associated with lower cardiovascular risk. I mean, that’s just incontrovertible at this point. If one doesn’t happen to have good genes, then, dietary control of cholesterol is also good, but hard to do. LDL cholesterol can be influenced by diet, but in someone who has really high LDL cholesterol, there’s a good chance that they would need medical therapy and certainly for secondary prevention, all those patients should be on LDL-lowering therapy and in high-risk primary prevention as well there’s a role for pharmacotherapy and by that I’m referring to statins and ezetimibe. With statins, many times a high-dose statin, high-potency statin will be needed, especially in secondary prevention. Ezetimibe is another great medicine, generic, underutilized. Really a shame. Very safe, not systemically absorbed, very rare to have side effects there.
And now the PCSK9 inhibitors. Expensive, yes, but highly effective at lowering LDL cholesterol and also lowering the rate of ischemic events. So really major advances there in terms of LDL control.
Can we do more beyond LDL control with respect to lipids? I think so. Are triglycerides a cardiovascular risk factor? I believe so. Specifically triglyceride-rich lipoproteins, but I’ll say triglycerides just for short. The Mendelian randomization work again supports that. In a paper that Brian Ference was a coauthor in JAMA, we looked at this and both LDL and triglyceride-rich lipoproteins were shown to be independent cardiovascular risk factors, but the degree of LDL change that was necessary to affect cardiovascular risk was much less than the degree of triglyceride change needed. If you believe that sort of Mendelian randomization work, which I do—I was coauthor of the paper and, obviously, I believe it—the implication is that for pharmacotherapy you would need to lower triglycerides by a lot to get the same reductions in cardiovascular risk that you see with LDL reduction. There are a bunch of different drugs that are being studied, things like small interfering RNA (siRNA) that lower triglycerides by an enormous degree. We’ll see if those agents lower triglycerides—do they lower cardiovascular risk? If the answer is yes, then the triglyceride hypothesis is proven. If the answer is no, then it’s disproven.
Having said that, though, we have icosapent ethyl, which I was studying in the REDUCE-IT trial, which was published in the New England Journal of Medicine a few years ago—a trial I was very involved with, there icosapent ethyl lowers triglycerides. REDUCE-IT was a trial of patients with elevated triglycerides. But the drug itself is eicosapentaenoic acid (EPA), an omega-3 fatty acid. While it lowers triglycerides, that’s probably not the predominant mechanism of benefit. That’s why the story about triglycerides can be a bit confusing. Drugs like fibrates have been shown not to be effective in statin-treated patients, even if they have elevated triglycerides. Omega-3 fatty acid supplements, mixtures of EPA and dehydroepiandrosterone (DHEA), have been found to be ineffective. But EPA… To date, all the trials have shown benefit, including REDUCE-IT. I think if there’s a patient with elevated triglycerides and they have had their LDL controlled, I think they should be on icosapent ethyl assuming there are no contraindications.
Beyond that, there are other drugs that are being tested. I recently had presented some data that were just published in Nature Medicine looking at an FGF21 analogue and in a phase 2 study that lowered triglycerides by about 50%, which I think is good. Beyond that, it also caused liver fat to melt away in just 8 weeks on magnetic resonance imaging (MRI). For anyone interested, the pictures are in Nature Medicine.
So triglycerides that are elevated, I think, carry independent cardiovascular risk. They’re also bad for our liver in terms of things like nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH). There’s some talk that name might get changed. To me, the triglycerides story isn’t totally over, but there’s enough evidence showing that it is atherogenic, that it is bad for the liver, that it is bad for cardiometabolic health, that I think treating it with evidence-based therapies is indeed useful. For now we do have icosapent ethyl that is evidence based and approved for that particular use in places like the USA and Canada.
Roman Jaeschke: You are using interchangeably eicosapentaenoic acid and icosapent ethyl acid, are those the same substances?
Deepak L. Bhatt: I’m glad you asked. Icosapent ethyl is a prescription medication. It is an ethyl ester of eicosapentaenoic acid. The active ingredient is EPA, but it’s at a high dose. It’s highly purified. If you were to take a supplement, for example, it’s not the same purity or the same concentration.
Roman Jaeschke: So if we wanted to prescribe it today, it would be icosapent ethyl acid?
Deepak L. Bhatt: Eicosapentaenoic acid, or EPA, is the active ingredient. The prescription drug name is icosapent ethyl and it’s available in the USA with multiple generics now. It’s available in Canada, where you have it as a branded drug, in Europe it’s a branded drug, it just got approved in China, so it’s available in many but not all regions of the world yet.
Roman Jaeschke: I suspect I will remeasure my triglycerides with that in mind. Professor Bhatt, it’s incredibly interesting for me as a clinician. I hope it will be interesting to our listeners. I really appreciate your time and I hope to invite you again if you didn’t find it too strenuous and time consuming. It was a great interview and I really appreciate it.
Deepak L. Bhatt: Yes, I really enjoyed the interview as well. Thank you so much.
Roman Jaeschke: Okay. Thank you and till next time.
Deepak L. Bhatt: All the best.
 English
English
 Español
Español
 українська
українська