Writing Committee, Drazner MH, Bozkurt B, et al. 2024 ACC Expert Consensus Decision Pathway on Strategies and Criteria for the Diagnosis and Management of Myocarditis: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2025;85(4):391-431. doi:10.1016/j.jacc.2024.10.080
Ammirati E, Moslehi JJ. Diagnosis and Treatment of Acute Myocarditis: A Review. JAMA. 2023;329(13):1098-1113. doi:10.1001/jama.2023.3371
Definition, Etiology, PathogenesisTop
Myocarditis is an inflammatory process involving cardiomyocytes, connective tissue, blood vessels, and sometimes also the pericardium. In the majority of cases etiologic agents cannot be identified. Apart from de novo infection, myocarditis can also be caused by reactivation of a latent infection.
Causes:
1) Viral infection (the most frequent cause; etiologic factors include parvovirus B19 [the most common etiologic factor of acute myocarditis with features similar to acute coronary syndrome, including diffuse ST-segment elevations], human herpesvirus type 6 [HHV-6], coxsackievirus B, adenoviruses, other herpesviruses, influenza, and SARS-CoV-2); bacteria (Borrelia burgdorferi, Mycobacterium tuberculosis, pneumococci, staphylococci, Haemophilus spp, Salmonella spp, Legionella spp), rickettsiae, mycoplasma, chlamydia, fungi (eg, Candida spp); protozoa (eg, Toxoplasma gondii, Entamoeba histolytica); parasites (eg, Trichinella spiralis).
2) Factors causing autoimmune reactions to allergens (tetanus toxin, vaccines, drugs), allogenic antigens (rejection of a heart transplant), autoantigens (systemic connective tissue diseases, eg, systemic lupus erythematosus; celiac disease).
3) Drugs and toxins: Antibiotics, antimycobacterial agents, antiepileptic agents, nonsteroidal anti-inflammatory drugs (NSAIDs), immune checkpoint inhibitors, diuretics, sulfonylureas, methyldopa, amitriptyline, clozapine, heavy metals, cocaine, excess catecholamines (pheochromocytoma), ionizing radiation, sodium azide, insect and snake venoms.
Clinical Features and Natural HistoryTop
1. Symptoms: Dyspnea caused by heart failure, chest pain caused by myocardial ischemia or coexistent pericarditis, palpitations.
2. Signs: Features of heart failure or pericarditis.
3. Manifestations characteristic for specific types of myocarditis:
1) Acute myocarditis: History of a recent viral infection. Prodromal symptoms characteristic of the infection (involving the upper respiratory or gastrointestinal tract) precede cardiac symptoms by several days or weeks. Myocarditis may mimic acute coronary syndrome with elevated troponin levels and normal results of coronary angiography. It is usually caused by adenovirus or parvovirus B19.
2) Eosinophilic myocarditis: Rash and peripheral eosinophilia. The most severe type (acute necrotizing eosinophilic myocarditis) can cause fulminant heart failure.
3) Giant cell myocarditis: Most frequently features of heart failure, including fulminant heart failure and cardiogenic shock. Arrhythmias, including ventricular tachyarrhythmias, as well as heart block are also commonly noted.
4. Classification of myocarditis based on its course:
1) Fulminant myocarditis: A sudden and clearly defined onset of the disease with rapidly developing heart failure, which may even progress to cardiogenic shock. Myocardial dysfunction resolves spontaneously or (less frequently) leads to death.
2) Acute myocarditis: A less clearly defined onset. In some patients left ventricular (LV) dysfunction may progress to dilated cardiomyopathy.
3) Subacute or chronic myocarditis: Progressive heart failure as in dilated cardiomyopathy.
DiagnosisTop
1. Laboratory tests: Increased erythrocyte sedimentation rate (ESR) (in 70% of patients); leukocytosis with neutrophilia (in 50% of patients) and C-reactive protein (CRP) (in 80%-95% of patients); severe eosinophilia in most patients with myocarditis in the course of parasitic infections, systemic vasculitis, or hypereosinophilic syndrome; elevated serum creatine kinase MB subunit (CK-MB) and cardiac troponin levels. Elevated CK levels are usually found in patients with acute or fulminant myocarditis or patients with acute exacerbation of myocarditis.
2. Electrocardiography (ECG) is usually abnormal, but ECG features are typically nonspecific. The most frequent findings include diffuse ST-T changes, ventricular and supraventricular arrhythmias, and atrioventricular conduction abnormalities, as well as Q waves, which are less frequent than in the case of myocardial infarction (MI).
3. Echocardiography is useful in the identification of patients with fulminant myocarditis, who usually have a nondilated LV with increased thickness and severe global hypokinesis. Other features in myocarditis can include regional wall motion abnormalities and preserved ejection fraction with diastolic dysfunction. The progression of heart failure is associated with features similar to dilated cardiomyopathy.
4. Magnetic resonance imaging (MRI) (Figure 3.14-1) reveals myocardial edema and a pattern of late gadolinium enhancement characteristic for myocarditis. MRI may also be helpful to exclude inflammatory and infiltrative etiologies, such as sarcoidosis, which has a characteristic pattern of patchy infiltration.
5. Endomyocardial biopsy is usually reserved for patients with life-threatening presentations, including cardiogenic shock with recurrent ventricular arrhythmias. In these situations biopsy may differentiate between specific etiologies of myocarditis, such as giant cell, lymphocytic, or eosinophilic myocarditis. If a diagnosis of giant cell or eosinophilic myocarditis is made, it helps guide immunosuppressive therapy to possibly reverse the underlying etiology.
Acute myocarditis should be suspected in young individuals with a sudden onset of heart failure, persistent arrhythmia or conduction disturbances, or with clinical features of MI accompanied by normal results of coronary angiography. In patients with symptoms of congestive heart failure and unclear onset of the disease, other causes of dilated cardiomyopathy must be excluded. The diagnosis of myocarditis is usually made based on a combination of the clinical presentation, laboratory testing, ECG, imaging studies (echocardiography, cardiac catheterization, and MRI), and, in some instances, endomyocardial biopsy.
Criteria for the clinical diagnosis of myocarditis (based on the 2013 European Society of Cardiology position statement):
1) Clinical presentations:
a) Acute chest pain, pericarditic or pseudoischemic.
b) New-onset (≤3 months) or worsening of dyspnea at rest or with exercise, and/or fatigue.
c) Subacute or chronic (>3 months) dyspnea at rest or with exercise, and/or fatigue.
d) Palpitation, unexplained arrhythmia, syncope, and/or aborted sudden cardiac death.
e) Unexplained cardiogenic shock.
2) Diagnostic test criteria:
a) Newly abnormal ECG (atrioventricular block or fascicular block, ST-segment elevation, T-wave inversion, ventricular tachycardia or fibrillation, asystole, atrial fibrillation, reduced R-wave height, intraventricular conduction delay [widened QRS], abnormal Q waves, low voltage, frequent premature beats, supraventricular tachycardia).
b) Elevated levels of troponin T or troponin I.
c) Functional and structural abnormalities on cardiac imaging (echocardiography, angiography, or cardiac MRI): New, otherwise unexplained LV and/or right ventricular structure and function abnormalities (including an incidental finding in apparently asymptomatic patients): regional wall motion or global systolic or diastolic function abnormality.
d) Tissue characterization by cardiac MRI: Edema or late gadolinium enhancement typical for myocarditis.
Myocarditis is clinically suspected if ≥1 clinical presentations and ≥1 diagnostic test criteria are found in a patient with excluded coronary artery disease or excluded other conditions that may cause similar symptoms (such as valve disease, congenital heart disease, hyperthyroidism). The higher the number of fulfilled criteria, the stronger the suspicion. In asymptomatic patients not fulfilling any clinical criteria, the presence of ≥2 diagnostic criteria is required (criteria 2a-2d) for the diagnosis of myocarditis.
Acute MI, sepsis, acute mitral regurgitation, tachycardia-induced cardiomyopathy and other causes of dilated cardiomyopathy, other causes of heart failure.
TreatmentTop
1. General measures:
1) Restricted physical activity, especially in the case of fever and other symptoms of systemic infection or features of heart failure. Patients should avoid strenuous or competitive exercise for 3 to 6 months.
2) Restricted alcohol intake.
2. In patients with chest pain and generalized ST-T changes suggestive of ischemia, you may use beta-blockers or amlodipine in low doses (to avoid lowering systemic blood pressure) as antianginals. In patients with mild systolic LV dysfunction, use angiotensin-converting enzyme inhibitors (ACEIs). In patients with pericardial involvement and normal LV function, colchicine and ibuprofen/aspirin could be used. NSAIDs should be avoided in patients with heart failure or shock.
3. Treatment of severe ventricular arrhythmia: Beta-blockers and antiarrhythmic agents may be used. However, short-acting beta-blockers (eg, esmolol) are preferred over longer-acting beta-blockers in the case of refractory ventricular arrhythmias because of the concern for worsening end-organ perfusion from their negative inotropic effect during a low-output shock state. In patients with bradyarrhythmias temporary cardiac pacing may be justified.
4. Treatment of heart failure: Standard management (see Heart Failure). In patients with fulminant myocarditis, restriction of physical activity, extracorporeal membrane oxygenation, and in some cases ventricular assist devices are used. Such patients should be urgently transferred to a center capable of mechanical circulatory support.
5. Heart transplant in patients in whom all other treatment modalities have been ineffective or patients with severe heart failure.
Treatment of Underlying Condition
1. Antimicrobial treatment is feasible in some viral infections (eg, herpes simplex virus) and in infections caused by other pathogens (eg, Borrelia spp).
2. Immunosuppressive treatment is effective in patients with myocarditis caused by systemic connective tissue diseases, sarcoidosis, hypereosinophilic syndrome, or in giant cell myocarditis.
3. Discontinuation of the offending drug with or without concomitant glucocorticoid treatment in patients with myocarditis caused by drug hypersensitivity.
PrognosisTop
Myocarditis has a current mortality rate of 1% to 7%. The majority of patients with acute or fulminant myocarditis recover completely. In a small proportion of cases a subclinical inflammatory process persists, leading to the development of dilated cardiomyopathy.The prognosis is poor in patients with subacute myocarditis. It is better in patients with a higher baseline LV ejection fraction and shorter disease duration. Adverse prognostic factors include New York Heart Association (NYHA) class III/IV heart failure at diagnosis and focal late gadolinium enhancement on MRI.
FiguresTop
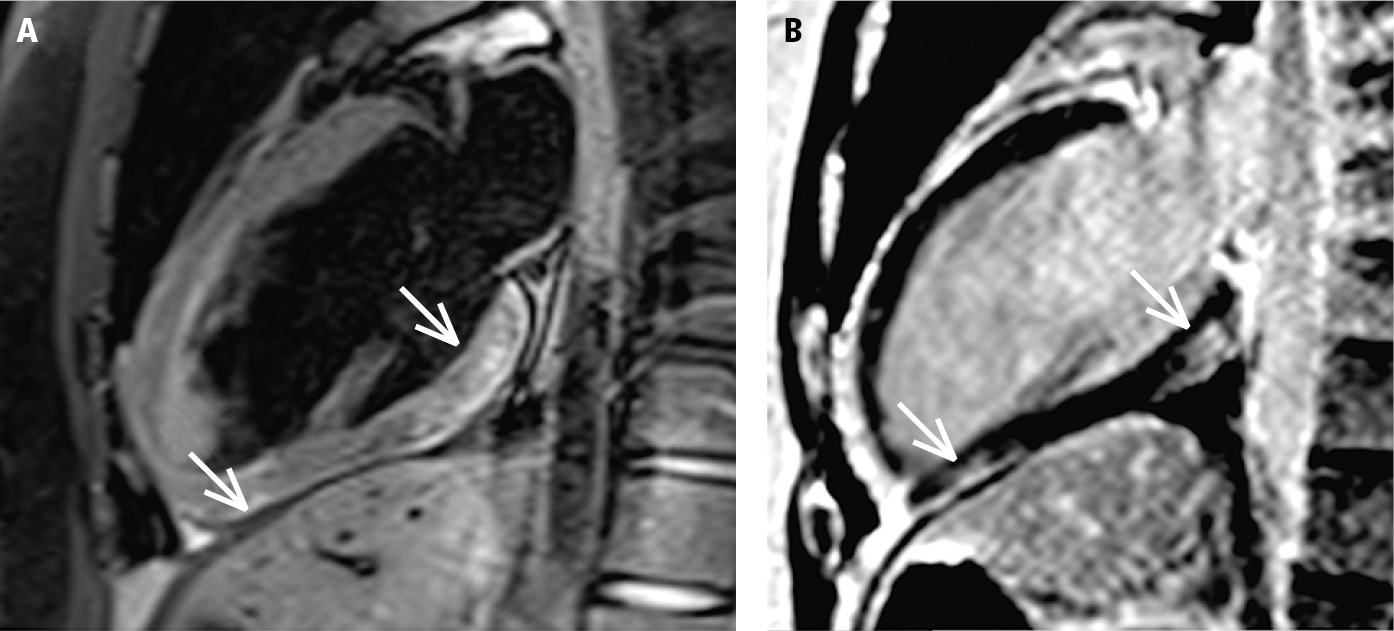
Figure 3.14-1. Cardiac magnetic resonance imaging (MRI) of a patient with suspected acute myocarditis, 2-chamber view. Both MRI criteria for acute myocarditis are met. A, features of myocardial edema (high signal intensity of the basal and apical inferior myocardial segments; arrows), the T2-dependent criterion. B, presence of the typical subepicardial late gadolinium enhancement in the area corresponding to the area of the edema (arrows), the T1-dependent criterion. Figure courtesy of Dr Łukasz Małek.