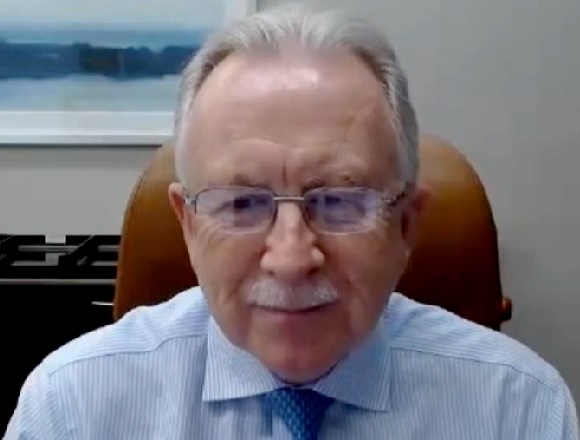
Kevin Woodward, MD, associate professor of medicine at the Faculty of Health Sciences, McMaster University, joins Roman Jaeschke, MD, MSc, DPharm, to discuss the resurgence of mpox, different clades of the virus, current treatments, and vaccination strategies.
Contents
- Mpox: Current epidemiologic situation
- Clade I versus clade II disease
- Treatment: Does TPOXX work?
- Prevention: Vaccination and risk groups
Transcript
Roman Jaeschke, MD, MSc, DPharm: Good morning, welcome to another edition of McMaster Perspective. I have a pleasure of having again Professor Kevin Woodward, a specialist in infectious diseases and sexual health.
We had an interview 2 years ago or so, when there was sudden interest in mpox—or monkeypox, as it was called—and Dr Woodward was a local and regional liaison for coordinating care for this suddenly appearing disease. We had a hiatus of almost 2 years and suddenly every time I open the news, there is mpox in it. Professor Woodward, why is it? What’s happening?
Kevin Woodward, MD: I think that back in 2022, when we had our first discussion, there was really that first outbreak of mpox that we saw in Canada, with almost 700 cases that occurred in Ontario. Then, as you said, we had this hiatus, right? In 2023 there were 30 cases. Now, what’s happened is there are actually 2 things going on.
Number 1, in Ontario at least, the number of mpox cases has been on the rise again. So, in the first half of 2024 we’ve seen ~100 cases of mpox diagnosed within Ontario. But this simultaneous thing that’s happened is a new outbreak of a different substrain of mpox called clade Ib, and this has happened in the Democratic Republic of Congo (DRC), where they’ve diagnosed >22,000 people with mpox or suspected mpox within that country. There have been cases within the neighboring countries, most recently a case was detected in Sweden, and then the World Health Organization (WHO) has declared an mpox outbreak and one of international concern.
So, we’re seeing these 2 different outbreaks, which are actually 2 different strains of the virus, but they’ve been happening at the same time and certainly, what I’m starting to hear about is, people are conflating them as being the same infection. What we’re seeing in Ontario is a continuation and a slight resurgence of that mpox that’s been going on since 2022. But also [there is] a new outbreak within the DRC at the same time.
Roman Jaeschke: So, the new outbreak, so to speak, present in—I think you were mentioning the DRC—these are theoretically or practically 2 different diseases and only one of them is really prevalent in Ontario at the moment.
Kevin Woodward: Yes, it’s 2 different strains of the virus. We call them clades of the virus. Most people are probably familiar with those phylogenetic trees of viruses. Clade I and clade II of mpox are causing different outbreaks. Clade I is the one that is present in the outbreak right now in the DRC and tends to be slightly more severe. Clade II is the one that’s been ongoing in Ontario since 2022 and tends to be less severe in terms of the symptomatology.
Roman Jaeschke: And no major number of cases or no cases of the more severe form in Ontario yet?
Kevin Woodward: That’s correct. We’ve had no… as I mentioned, there’s been one case of clade I that’s been detected in Sweden. I think that was just last week. But other than that, they haven’t detected any within Europe and certainly not in the United States or Canada. We’ve had clade II that’s been local transmission ongoing since 2022.
Roman Jaeschke: And slightly increasing.
Kevin Woodward: Yeah. I mean, the question is, will we see clade I disease in Canada? I think from what the history of epidemics has told us, we probably will. Hopefully with this increased surveillance, we’ll be able to isolate and prevent transmission of that happening locally.
Roman Jaeschke: How do they differ clinically? Could you remind us? You see half of the cases in Ontario, I understand. How do they differ? How can we differentiate? What can we expect from either of them?
Kevin Woodward: In mpox in general, you tend to get the pox-like lesions. For clade II, what we’ve been seeing in Ontario is anogenital lesions. They can be quite painful usually around the anus, the genitalia, and sometimes around the mouth, and it tends to be spread by sexual contact. In the clade I disease that we’re seeing in the DRC, the patients tend to have more lesions, although we are seeing some sexual transmission with the clade Ib disease—that’s the current outbreak—as well as household transmission.
I think epidemiologically the other thing that’s different is within the current outbreak in the DRC is we’re seeing a lot more children who are being infected, probably by household contact. Indeed, those children are the ones who tend to have more severe disease, so, much more disseminated disease, whereas in adults, the mortality rate has been lower and overall the disease tends to be a little bit less severe. But in general we think of clade I as more severe disease with a higher mortality rate, more lesions, more discomfort. Clade II tends to be less severe.
Roman Jaeschke: What kind of mortality rate are we talking about?
Kevin Woodward: In the current outbreak in the DRC, I think it’s been reported ~3%, but the majority of that has been in children aged <15 years.
Roman Jaeschke: Ok, now treatment. I remember we were talking about some availability of treatments 2 years ago. Anything changed?
Kevin Woodward: Not really. We talked about TPOXX, which was the antiviral that was available 2 years ago that we were using for emergency cases that’s still available now through the Health Canada special access [program]. I think that the thing that we still don’t know—and there are trials for this, which are ongoing even here in Toronto—is, does it actually work? As I’m speaking to you, one of the fathers of evidence-based medicine, anecdotally, it works. We have no randomized controlled trials [editor's note: see the latest news release on the unpublished results of the PALM007 trial performed in the DRC: LINK]. There is a trial that’s ongoing right now that is actually looking for participants within Ontario, but what we’ve seen anecdotally is some people get a lot better and then some people don’t. So, if you asked me, back of the napkin, if I had a bad case of mpox, would I want TPOXX, I’d say sure, because I think we’ve not seen a lot of side effects from it. But at the same time, I have no clue if it actually really makes a difference.
Roman Jaeschke: That would be important. How about prevention? What can we do?
Kevin Woodward: Vaccine. We have a vaccine available in Canada for those individuals right now who are at risk. That’s generally gay, bisexual, and other men who have sex with men (GBMSM). They should go and get vaccines. In the recent resurgence of cases that we’ve had in 2024, almost 70% of those have been in unvaccinated individuals. And what we see from literature since 2022 is that although getting your 2 doses of your smallpox IMVAMUNE vaccine, which protects against mpox as well, doesn’t give you 100% protection from getting mpox a second time, it does tend to be much less severe if people have had their doses of vaccine. So, for those individuals who are at risk for the current Ontario outbreak, we would recommend going and getting that vaccination, and getting it as soon as you can, and really trying to get the second dose—for people who only had one dose maybe in 2022 and this happened, go ahead and get the second dose. There are questions around how long the immunity lasts for; do you need booster doses? All of those questions are still up in the air, right now that’s not being recommended, but certainly if you’ve not been vaccinated, go out and get a vaccine.
Roman Jaeschke: Just to clarify, is this a specific vaccine for mpox?
Kevin Woodward: It’s a vaccine that was developed for smallpox but has been shown to provide immunity for mpox as well. Smallpox and mpox are very closely related viruses. We don’t have a specific mpox vaccine that we use in Canada.
Roman Jaeschke: Right. So this is a fairly standard old-time vaccine developed decades ago, correct?
Kevin Woodward: The one that we’re using in Canada, which is IMVAMUNE, is a newer version of an old smallpox vaccine.
Roman Jaeschke: Ok. So, generally speaking, I believe you provided me with very relevant information. We are not dealing [with clade I mpox]—in Canada at least or outside the one case in Sweden—the cases seem to be confined to the DRC and surrounding countries. There is some treatment of unknown efficacy yet and you are conducting a study, I suspect, as you mentioned; and there is a reasonable, if not a good vaccine, which people, especially people at risk, should be taking. Should the general public consider this vaccine regardless of the presence of risk factors?
Kevin Woodward: No. What we’ve seen for the current clade IIb outbreak that we’re having in Ontario that’s ongoing is, it’s been almost exclusively amongst GBMSM. We also don’t have enough vaccine supply to vaccinate the general public. So, right now we are recommending it only for those people who are within those specific risk groups to go and get a vaccine.
Roman Jaeschke: OK. I hope that we’ll have another 2-year hiatus because somehow the outbreak will slow down and die out. Thank you very much, Professor Woodward. Appreciate and appreciate all your work with this disease. Thank you.
Kevin Woodward: Happy to chat.
 English
English
 Español
Español
 українська
українська