Ashkan Shoamanesh, MD, associate professor of medicine at McMaster University who holds the Marta and Owen Boris Chair in Stroke Research and Care, meets with James Douketis, MD, expert in thromboembolic diseases, to share an overview of treatment approaches for patients who developed intracerebral hemorrhage while using anticoagulants, contextualizing their discussion with insights from the ANNEXA-I trial.
For a Publications of the Week article discussing andexanet in DOAC-treated patients with intracerebral hemorrhage, click here.
Contents
- Incidence of ICH in patients receiving anticoagulation
- ICH: Severity and consequences
- Brain injury after ICH
- Acute ICH: Blood pressure control and stopping hematoma growth
- Hemostatic treatment and reversal agents after ICH
- What’s new? Clinical trial data on andexanet alfa
Transcript
James Douketis, MD: Hello everyone. My name is Jim Douketis and I’m pleased to welcome you to another edition of the McMaster Textbook of Internal Medicine Publications of the Week—McMaster Perspective.
I’m delighted to welcome Dr Shoamanesh to this session. He is associate professor in the Department of Medicine and holds the Marta and Owen Boris Chair in Stroke Neurology, and he was a co-author of the paper that we will be discussing, on the ANNEXA-I trial, which looked at a reversal agent for patients who were receiving an oral factor Xa inhibitor anticoagulant and suffered intracranial hemorrhage (ICH). Welcome, Ashkan, and thank you again for your perspective.
I want to just maybe step back a bit and look at the issue of ICH. This is probably the most feared complication of anticoagulant therapy, and maybe you can just give us a little background on how common it is and how severe it is. What’s the prognosis of this outcome?
Ashkan Shoamanesh, MD: Yeah, for sure. Thanks so much. I’ll begin by saying thank you for having me and the opportunity to chat with you today on behalf of the ANNEXA-I investigators and particularly Stuart Connolly, who is the trial Principal Investigator (PI).
ICH, as you pointed out, is a disease that I’m happy to see is getting more and more attention because there is a major unmet need in improving the outcome of this grave disease population. Currently in the Western Hemisphere, the incidence of ICH is ~15 to 20 per 100,000 individuals. In Canada it is just ~15 per 100,000, however, it can be as high as 100 per 100,000 individuals in high-incidence regions, such as Southeast Asia. Unfortunately, as is common in many other cardiovascular diseases, the burden of disease is greatest in low- and middle-income countries, so there is some global disparity regarding the impact of ICH.
When it comes to what is the rate in people who are already on anticoagulation, which is going to be kind of the focus of our discussion a bit later, it’s ~1% for patients who are on vitamin K antagonists for atrial fibrillation and that is halved in patients treated with direct oral anticoagulants (DOACs). So, in the latter group, the incidence is ~0.4% per year in patients who are on novel oral anticoagulants (NOACs). Actually one of the reasons NOACs have become favored over vitamin K antagonists, apart from their ease of use and lack of blood monitoring, is really the halving of ICH with these agents compared to traditional vitamin K antagonists.
And in terms of the severity, well, it’s quite grave. Although it accounts for only about a third of all strokes, ICH accounts for about half of the global burden of death and disability from stroke. Some ballpark numbers [suggest] that there is ~25% 1-month mortality, which can go up as high as 55% at 1 year in people on anticoagulants. These patients have a 35% chance of having progressive cognitive decline after their stroke and close to half will have unfavorable outcomes at the time of discharge. The only silver lining with ICH is that the functional trajectory, if you do survive, tends to be a bit better than in ischemic stroke, and that you can be quite disabled initially, but if you survive your hospitalization, you do have continued improvement up to ~1 year post stroke, whereas in ischemic stroke patients, typically their recovery plateau is ~3 to 6 months.
James Douketis: OK, thank you. I think we all recognize this is a devastating illness and complication. Now, let’s consider how to manage these patients. You are an internist and you have one of these patients come to your emergency room (ER). Maybe I can have a 2-part question for you.
The first is that if, let’s say, you don’t have any reversal agent at your disposal, how would you manage these patients? Is there any role for the administration of prothrombotic, prohemostatic agents like tranexamic acid (TXA)?
The second part is, what about andexanet alfa? Does that add something to our therapeutic armamentarium? Please feel free to talk about the trial: some of the key strengths and perhaps some of the key weaknesses.
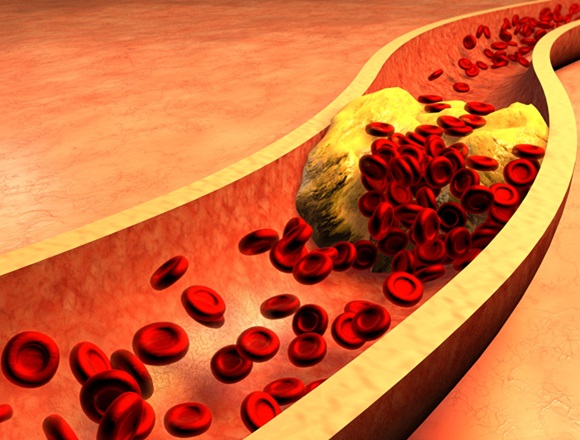
Ashkan Shoamanesh: Sure. As we think about the management of acute ICH, there are really 2 waves of brain injury that can occur in ICH as part of pathophysiology. The first is primary structural injury to the brain, and that’s really from the rapidly expanding hematoma. As it’s growing, it’s tearing axons and compressing surrounding neurons, causing death of these cells. In addition, there’s a wave of inflammation as heme-mediated toxicity occurs. As macrophages come in, they start degrading—or digesting, I guess—the heme and then that leads to reactive oxygen species (ROSs) being released, increased blood-brain barrier permeability. Thrombin generation can actually increase blood-brain barrier permeability as well, and that can [cause] the second wave of injury. But ultimately, what drives both is the size of that hematoma, right? The larger the hematoma, the more damage to surrounding tissue and the larger the hematoma, the more red blood cells that would be there, and the more heme-mediated toxicity. Thus, really, the Holy Grail of acute ICH treatments, apart from, of course, ensuring the ABCs in that patient, and that intracranial pressure (ICP) is being well controlled, and so forth, is trying to mitigate the hematoma growth. That’s really the primary target of our treatments.
And one way we do that in all-comers, irrespective of whether they’re on anticoagulants or not, is blood pressure control. And there’s increasing evidence that really a target of <140 mm Hg for systolic pressure is what we should be aiming for as soon as possible after an ICH, as long as we’re not dropping the systolic pressure by >60 mm Hg. So, you get <140 mm Hg, to a 120 to 140 mm Hg range. That should be your goal unless you need to drop them from like 220 mm Hg to get there, because then you’re surpassing that 60 mm Hg delta. And then the next piece, of course, to try to mitigate a secondary inflammatory brain injury and also a bit of the primary injury, is hematoma evacuation procedures. They haven’t really gained much prominence except for large bleeds in the cerebellum, where we’re pretty comfortable going with posterior or suboccipital decompressive craniectomy. And then, of course, we can use intraventricular drains for people with hydrocephalus.
Now, there’s a trial that was recently published, called the ENRICH study, which shouldn’t be confused with ENRICH-AF, which is another study we’re leading at McMaster. The ENRICH study looked at minimally invasive hematoma evacuation in patients with acute ICH within 24 hours of symptom onset. And in those with lobar ICH, there was benefit. With that procedure, we may start seeing more hematoma evacuation on the basis of those results.
When it comes to hemostatic treatments, or reversal agents, there are 2 scenarios, of course. The first is the patient that’s not on an antithrombotic agent and there we don’t have any definitive evidence yet, but we are exploring things like TXA and recombinant factor VII in ongoing trials. There have been some signals of efficacy in secondary outcomes and subgroup analysis with TXA. For instance, myself, sometimes I will still use TXA in a spontaneous ICH because (1) it’s cheap, (2) it doesn’t seem to be harmful; it doesn’t seem to have any thrombotic complications associated with it. So, if someone is presenting really early in their ICH or the imaging features of their ICH suggest that it’s a person who’s at high risk of expansion, I may still use it, however, accepting that I don’t have good evidence to back up my decision making, but there is some suggestive evidence in the literature so far that we’re now trying to confirm in additional trials. Beyond that, there’s really no basis or role for hemostatic treatments in someone who’s not on an antithrombotic agent.
Interestingly, if someone is on an antiplatelet agent, there was the PATCH study that suggested that actually giving platelet transfusions causes harm and we don’t know exactly what that was due to, but it may be because of that excess thrombin generation causing some of that secondary brain injury, or it may also be that platelets release a bunch of cytokines that could exacerbate inflammation and blood-brain barrier permeability, so platelet transfusions are not recommended in people on antiplatelet agents.
And then, when it comes to anticoagulants, that’s really when reversal agents and hemostatic therapies are being used. In patients who are on vitamin K antagonists really the standard of care for some time now has been giving a 4-factor prothrombin complex concentrate (PCC) with vitamin K at a dose of 10 mg IV. That really replaced fresh-frozen plasma (FFP), which was what we were using historically, based on how rapidly PPC is able to reverse the international normalized ratio (INR) relative to FFP. In the FFP days, we had to wait several hours, often 5 to 6 hours, to get to an INR <1.2, whereas with PCC we can do that much more rapidly.
Now, for dabigatran, which is a direct thrombin inhibitor, we have idarucizumab, and that’s a direct reversal agent that’s now widely being used in Canada. For heparin, although we don’t have hard data from randomized trials, particularly on ICH, we do use protamine, and even if it’s unfractionated or fractionated heparin, there is a theoretical role for protamine.
Then, when it comes to the bulk of our discussion today, and that’s going to be patients who are on factor Xa inhibitors, that’s where at present the standard of care and guidelines in Canada are using a 4-factor PCC. And in our Canadian stroke practice recommendations, we recommend 50 IU/kg up to a maximum of 3000 IU for the reversal of factor Xa inhibitor–related ICH. However, it’s important to realize that there isn’t much data that supports that PCC can benefit patients, particularly in the setting of acute ICH, and that 50 IU/kg dose comes from a punch biopsy study, where in patients treated with 1 dose of edoxaban 60 mg, getting 50 IU/kg up to a maximum dose of 5000 IU—mind you, not the 3000 IU that we use in clinical practice—and as you can imagine, the majority of patients being 70 kg, the majority of patients in that study had gotten doses higher than the 3000 IU maximum that we use in clinical practice. The 50 IU/kg dose of PCC led to reduced bleeding times and decent timing to normalization of endogenous thrombin potential (ETP) and that person’s capacity to build thrombus—thrombin rather—and by extension, clot, and that was ~1 to 1.5 hour.
Still, for an acute ICH, that’s too late and many other studies suggest it takes ~6 hours to reverse or normalize ETP with 4-factor PCC. Another thing to keep in mind, before we get into ANNEXA-I results, is that all the studies that have looked at… there haven’t been many, but all the ones that have looked at the effect of PCC on anti–factor Xa activity as a measure of whether it’s actually having an effect on the factor Xa inhibitors’ direct role show absolutely no relationship whatsoever and that PCC behaves the same as saline. And really the reason for that is that factor Xa inhibitors provide 1:1 stoichiometric inhibition to factor Xa and you really need very large concentrations of factor X to compete against those factor Xa inhibitors. There simply isn’t enough factor X in 4-factor PCC to overcome that level of inhibition. You would have to give exceedingly large doses that are just not being used in clinical practice to do that. This is why we don’t see an effect on anti-factor Xa activity, but for whatever the reason, PCC does have this bypassing effect where we do see some normalization of ETP relative to nothing in healthy volunteer studies of patients receiving factor Xa inhibitors. But typically that’s delayed.
On the other hand, we already know from studies like ANNEXA-4 and some of the early andexanet studies led out at McMaster by Stuart Connolly and Deb Siegal—Mark Crowther, of course, was a big part of that as well—and what those studies showed is that with andexanet alfa you get immediate reversal of ETP and it’s sustained. You also get immediate reduction in anti–factor Xa activity. And although there’s a bit of a rebound of anti–factor Xa activity after the end of the bolus—sorry, after the end of infusion rather—the ETP, once it’s normalized, it’s maintained and [there is] sustained normalization of ETP.
This background or framework leads us into ANNEXA-I and on the basis of the ANNEXA-4 study, where… it was a single-arm study similar to the idarucizumab study, there was a conditional approval obtained for andexanet alfa in Canada, but it was never actually funded by any of the funding systems or hospitals. And in that ANNEXA-4 study what they showed was that the rate of hematoma expansion in ICH patients was only ~20%, which is much better than the 40% you would expect in patients who aren’t treated with a reversal agent. But the rate of thrombotic events was also 10% and a bit higher than what you would expect. And because it was a single-arm study, there was no way of knowing whether or not those findings were actually treatment effects of andexanet alfa or just a reflection of the underlying population that got into this study. As a conditional approval of andexanet alfa, regulatory bodies in the United States, European Union, and Canada mandated a randomized controlled trial (RCT) in a severe bleeding situation and this is where ANNEXA-I comes in.
ANNEXA-I was a phase 4 study. It was a prospective, open-label, blind randomized trial where patients who presented with acute ICH within 6 hours of symptom onset, who had taken their factor Xa inhibitor dose within 15 hours of randomization and who had hematoma volumes ≤60 cm3, were randomized 1:1 to receive andexanet alfa versus usual care. The primary efficacy outcome was basically termed a hemostatic efficacy and it had 3 components that had to be met. All 3 had to be met: (1) ≤35% growth of the hematoma from baseline computed tomography (CT) imaging to 12 hours, (2) <7-point increase in the score on the National Institutes of Health Stroke Scale (NIHSS) from baseline to 12 hours as a measure of acute neurologic deterioration, and (3) no rescue therapies between 3 and 12 hours after randomization. This study was originally planned to have a sample of 900 participants to show a difference in this primary efficacy end point; however, after ~450 individuals underwent an interim analysis—and this was a prespecified interim analysis—the Data and Safety Monitoring Board (DSMB) asked that the study be stopped and a big driver of that decision was overwhelming efficacy for reducing hematoma expansion—or increasing hemostatic efficacy rather—with andexanet alfa versus usual care. Ultimately, by the time the interim analysis occurred and the decision was made to stop the study, another 80 participants got into the study, so the extended population is 530 patients in total.
The secondary efficacy end points included looking at the change in anti–factor Xa activity from baseline to nadir, and that was measured at 2 hours, and then safety outcomes included thrombotic events and mortality. The overall trial results were that for every 100 patients treated, 13 people were less likely not to meet the hemostatic efficacy primary end point, so the number needed to treat (NNT) was <10 to have greater hemostatic efficacy with andexanet alfa versus usual care. In the usual-care arm, it’s worth noting that 87% of the population received PCC and the majority, >90%, was given 4-factor PCC, and that the median dose was 3000 IU—the maximum dose that’s recommended for reversal of factor Xa inhibitors in current guidelines in Canada. It was, we feel, an adequate comparison against what guidelines are currently recommending.
When we look at other end points, for instance, the effect of andexanet alfa on anti–factor Xa activity, there was ~97% reduction with andexanet alfa versus ~25% reduction with usual care. Again, that 25% or 27% reduction is what you would expect with saline based on health-care volunteer studies. It’s basically just a natural clearance of factor Xa inhibitors. And then, interestingly, when we looked at subgroup interactions for this primary efficacy end point, we found a couple of things to note. The first was that although the effect of andexanet on anti–factor Xa activity was a bit less in edoxaban-treated patients because of the greater biological distribution of edoxaban, the effect on the primary end point of hemostatic efficacy was essentially no different; it was the same irrespective of the NOAC you were on. The second thing to note is that when you looked at the primary efficacy end point, the effects of andexanet versus usual care were really no different whatsoever if someone was receiving PCC as part of usual care or not, and if anything, numerically the numbers were going against receiving PCC, but that was likely a chance finding or perhaps a bit of a patient selection bias in those who were deemed to ultimately receive PCC as part of usual care versus not. And although this isn’t the perfect comparison, particularly because the no-PCC group was small, only 15% of the overall population, and because there are none random reasons why someone may have ultimately received PCC as part of usual care versus not, when I combine that point with the fact that the 40% to 50% expansion rate that was seen in PCC was essentially what you would expect from historical controls in people who received nothing in this context, the lack of effect of anti–factor Xa activity from PCC and the fact that the healthy volunteer ETP data suggest that if it does make a difference, it’s in a delayed fashion, at least an hour or even greater in many studies, it really leads me to question whether PCC provides any benefit at all in a time-dependent closed-space situation like ICH. The majority of ICH expansion occurs within the first 3 hours and patients are presenting to the hospital on average ~2 hours after symptom onset. So you really have a golden hour to get that person’s coagulation normalized before being able to mitigate hematoma growth, and I just don’t think PCC is well suited for that task. This is why we may not be seeing any difference whatsoever between those who receive nothing versus those who receive PCC as part of usual care. Mind you, there is a bunch of limitations to interpretation of that subgroup that I already outlined.
We also looked at a clinical end point of modified Rankin Scale (mRS) at 30 days. The problem with this outcome, and this was a neutral finding: there was no difference between either group in terms of looking at functional independence of mRS ≤3 or, sorry, good outcome—not really functional independence because at 3 you have some level of dependency—so, good outcome of mRS ≤3, and this was a neutral finding, but it’s worth noting that (1) we never had power for this finding, or for this outcome rather, even when we had an initial sample size of some of 900 participants, and certainly we didn’t have any power for this once we got stopped early at 530 participants, and (2) the 30-day window is just way too early. As I mentioned to you at the beginning of this conversation, ICH patients look like crap initially, and it’s only after 6 to 12 months of follow-up that they recover. So, really, we’ve never seen acute treatments differentiate themselves in terms of impact on clinical outcomes in acute ICH studies until we went out to 6 to 12 months. And we’ve definitely never seen anything at 30 days. So I just think that the limitations of power and early assessment of that outcome, unfortunately, do not help inform the decision here. It doesn’t help us in either way. It’s just an inconclusive finding that has no bearing on our interpretation of results, unfortunately. That’s why one of the limitations of the study is that really it wasn’t well designed to capture these more clinical end points that people have wanted to see. And this is the reasoning for that. I wasn’t there at the time that the primary end point was decided, but it was actually a regulatory decision that was made between the company, Stuart Connolly, and the United States Food and Drug Administration (FDA). This is what the FDA wanted and the trial delivered what the FDA wanted because they just wanted to show that the drug was doing what it was meant to do and stop bleeding.
Then, because we didn’t have that end point, we tried to get around that by looking at a more strict definition of hematoma growth, and that’s ≥12.5 cm3, and seeing in how many does andexanet prevent the growth ≥12.5 cm3 because that threshold has a 80% positive predictive value of poor functional outcome at 90 days in the literature and we did find that for every 100 patients treated, ~6 were more likely to have less growth at that threshold, which we think is clinically relevant.
Then, when we looked at safety end points, the benefit of andexanet alfa was partially offset in that for every 100 patients treated, 5 were more likely to have a thrombotic event, so the number needed to harm (NNH) was ~20. If you look at ICH patients in isolation, and you exclude subdurals and you exclude epidurals and subarachnoids, the NNH is ~25 for thrombotic events, and concerningly the majority of this was driven by ischemic stroke, which of course has more clinical relevance than thrombotic events like deep vein thrombosis (DVT) and pulmonary embolism (PE). Then, there was a neutral finding in mortality. But again, the mortality end point was just not powered even when we had 900 patients, let alone when we got stopped early at half that size.
And then, when we looked at subgroup interactions for the thrombotic event outcome, what was interesting and, although there were no significant subgroup interactions, there was a numerical trend that suggested that the majority of excess thrombotic events with andexanet occurred in those who had a prior arterial thrombotic event, a myocardial infarction (MI) or ischemic stroke, and although statistically the interpretation is that this is a neutral finding, when you add the biological plausibility—a pretty good biological plausibility that those who’ve already had a thrombotic event bear greater risk of thrombotic events with this drug—it does suggest that perhaps if you exclude patients that had a prior arterial thrombotic event, you can maximize the benefit and minimize the harm. That was, I guess, the big take-home point from the study.
Andexanet alfa does have a conditional approval with Health Canada. Right now Astra Zeneca is trying to change that to a full approval. At present, with the empowerment of the ANNEXA-I data, it’s trying to get hospitals to fund the drugs so we have it on the shelves. I think what it really comes down to is that we have been in this situation before, right? Of course, all of us would have wanted to see an adequately powered trial that showed a difference in mortality and clinical end points, and unfortunately, for historical reasons, we don’t have that study, right? But this is the data we do have and we need to make the best of it. And it’s not like we’ve never been in a situation where we had to balance competing risks and benefits. For instance, the alternative of anticoagulation is the other thing, it’s basically where we’re trying to reduce thrombotic events at an increased risk of bleeding events, and now we’re in a situation where we’re trying to reduce bleeding events at an excess cost of thrombotic events, but fortunately the NNT is half the NNH. So, overall, as long as the weighting of hematoma expansion, as far as clinical consequences go, is the same as of thrombotic events, one could reasonably assume there would be net benefit there. We went through that exercise and we just presented that data at the European Stroke Organisation Conference (ESOC)—one of our Swiss colleagues, David Seiffge, presented this data—and we looked at—as best as we could in an adjusted model—what was the independent contribution of hematoma expansion to mortality and poor outcome in this study, and what was the independent contribution of a thrombotic event to death and poor outcome, and indeed there were more or less the exact same, and if anything, for functional outcome, hematoma expansion may have been a bit more relevant. So, a conservative take on that data is that they can be weighted equally, so that the NNT and NNH can be taken as a 1:1 trade-off and that the numbers suggest overall net benefit from andexanet when going through that exercise.
James Douketis: Ashkan, I got to thank you for a real tour-de-force overview of the ICH, the management options, and your behind-the-scenes perspective of the ANNEXA-I trial.
I think my takeaway is that this is a potentially beneficial drug when used selectively at the right time in the right patient, and it seems like this is not the end of the story and that we’re going to need to do further studies. And we welcome to hear more about the research you and your colleagues are doing. Thank you very much once again for providing your perspectives for the McMaster Textbook of Internal Medicine. Thank you.
Ashkan Shoamanesh: Thanks, Jim.
 English
English
 Español
Español
 українська
українська