No benefit of aspirin in the elderly without CV disease
McNeil JJ, Wolfe R, Woods RL, et al; ASPREE Investigator Group. Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly. N Engl J Med. 2018 Sep 16. doi: 10.1056/NEJMoa1805819. [Epub ahead of print] PubMed PMID: 30221597.
McNeil JJ, Woods RL, Nelson MR, et al; ASPREE Investigator Group. Effect of Aspirin on Disability-free Survival in the Healthy Elderly. N Engl J Med. 2018 Sep 16. doi: 10.1056/NEJMoa1800722. [Epub ahead of print] PubMed PMID: 30221596.
Elderly patients without cardiovascular disease and without dementia or disability do not benefit from a regular intake of acetylsalicylic acid (ASA).
Between 2010 and 2014, over 19,100 community-living independent adults without cardiovascular disease entered a study in which they received either 100 mg of aspirin daily or placebo.
After a median follow-up of 4.7 years, the risk of death from any cause was 12.7 events per 1000 person-years in the ASA group and 11.1 events per 1000 person-years in the placebo group (5.9% vs 5.2%; hazard ratio [HR], 1.14; 95% CI, 1.01-1.29). This difference was related to an unexpectedly higher risk of cancer-related deaths in the ASA group: 1.6 excess deaths per 1000 person-years (3.1% vs 2.3%; HR, 1.31; 95% CI 1.10-1.56).
During the same period, the risk of cardiovascular disease was 10.7 events per 1000 person-years in the ASA group versus 11.3 events per 1000 person-years in the placebo group (4.7% vs 4.9%; HR, 0.95; 95% CI, 0.83-1.08). The corresponding risk of major hemorrhage was 8.6 versus 6.2 events per 1000 person-years (3.8% vs 2.8%), respectively. There was no difference in the rate of persistent physical disability (1.8% vs 2.2%; a secondary end point) and in the risk of death from any cause, dementia, or persistent physical disability (9.7% vs 9.5%; HR, 1.01; 95% CI, 0.92-1.11; the primary end point).
Overall those results indicate no clear benefit of ASA in healthy elderly adults without cardiovascular morbidity.
Prophylactic aspirin in diabetes mellitus
Should patients with diabetes mellitus (DM) receive prophylactic acetylsalicylic acid (ASA)?
Over the course of 7.4 years, over 15,400 patients with DM and no history of cardiovascular disease received daily either 100 mg of aspirin or placebo. The mean age of patients in both groups was 63 years.
The frequencies of events in the ASA group versus the placebo group were as follows: for nonfatal ischemic stroke, 2.6% versus 3.0%; for transient ischemic attack (TIA), 2.2% versus 2.5%; for nonfatal myocardial infarction, 2.5% in both groups. The frequency of any serious vascular event or revascularization was 10.8% versus 12.1%, respectively (rate ratio, 0.88; 95% CI, 0.80-0.97).
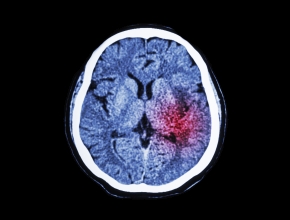
Bleeding classified as major occurred more commonly in the ASA group than in the placebo group at a rate of 4.1% versus 3.2%, respectively, with intracranial bleeding occurring in 0.7% versus 0.6% of patients and serious gastrointestinal bleeding, in 1.8% versus 1.3%. There was no difference in rates of gastrointestinal tract cancers or all cancers.
The authors interpret those results as indicating a balance between the risks and the benefits of using ASA in patients with DM.
Restrictive vs liberal transfusion strategies for cardiac surgery
Another instance in which a restrictive transfusion strategy was not worse than a liberal one (see Restrictive vs liberal fluid therapy in major abdominal surgery from Publications of the Week, May 28).
In this study over 5200 patients undergoing cardiac surgery were managed according to either a liberal red-cell transfusion strategy (threshold for transfusion, 95 g/L) or a restrictive strategy (threshold for transfusion, 75 g/L).
After 6 months of follow-up, death occurred in 6.4% of patients in the liberal strategy group versus 6.2% in the restrictive strategy group. Stroke occurred in 3.3% and 4.0% of patients, respectively; new-onset renal failure, in 4.2% versus 3.9%; and myocardial infarction, in 7.3% of patients in both groups. These individual differences were not significant, and neither was the difference between their combinations.
 English
English
 Español
Español
 українська
українська