Internal Medicine Rapid Refreshers is a series of concise information-packed videos refreshing your knowledge on key medical issues that general practitioners may encounter in their daily practice. This episode reviews the key aspects of the management of diabetic ketoacidosis.
Contents
- Introduction
- Pathophysiology
- Clinical presentation and diagnosis
- Management
- Management: Hemodynamic instability
- Management: Electrolyte abnormalities
- Management: Anion gap metabolic acidosis
- Management: Hyperglycemia
- Management: Identification and treatment of the precipitating cause
- Management: Other
- Credits
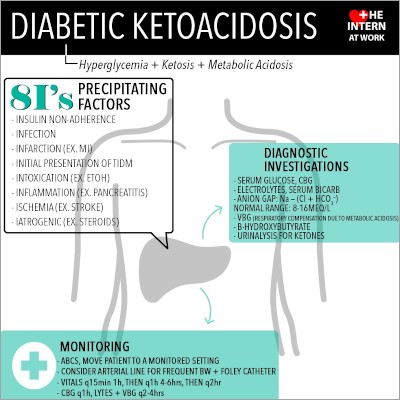
Infographic
Click to view the full image.
Infographic courtesy of The Intern at Work (theinternatwork.com).
Useful links
- Chapter on diabetic ketoacidosis from the McMaster Textbook of Internal Medicine
- 2018 guidelines for the prevention and management of diabetes by Diabetes Canada
- Anion gap calculator at mdcalc.com
Transcript
Introduction
I’m Heather Bannerman, a senior medical resident at McMaster University. This Rapid Refresher video will describe a practical approach to diagnosis and management of diabetic ketoacidosis (DKA). It is targeted to independently practicing subspecialists who are returning to general internal medicine and who want to brush up on their knowledge. This is not meant to serve as medical advice to the general population.
Pathophysiology
DKA is a state of insulin deficiency and excess counterregulatory hormones (glucagon, catecholamines, cortisol, growth hormone). It is often triggered by patients decreasing or omitting their insulin doses as well as other precipitants, which will be discussed later. This leads to osmotic diuresis, dehydration, electrolyte abnormalities, hyperglycemia, and an elevated anion gap metabolic acidosis related to both increased ketones and, not infrequently, lactate.
Clinical presentation and diagnosis
There are a wide variety of presenting signs and symptoms, as listed on the screen. Kussmaul breathing refers to a pattern of rapid and deep breathing followed by shallow breaths. There may also be signs and symptoms related to the underlying precipitating cause of DKA.
The diagnosis of DKA is made based on an elevated anion gap metabolic acidosis with elevated serum ketones and hyperglycemia. An anion gap >12 indicates an elevated anion gap, and this should be adjusted for albumin level, as hypoalbuminemia can underestimate the anion gap. There are online calculators that can do this for you (eg, at mdcalc.com).
Even though hyperglycemia was mentioned as part of the diagnosis of DKA, some patients may present with a “euglycemic DKA.” These patients include those on sodium glucose contrasporter-2 (SGLT2) inhibitors (eg, empagliflozin), as well as the others listed on screen the screen (patients with pregnancy, prolonged fasting, severe cirrhosis, or acute alcohol ingestion). Consider other causes of elevated anion gap metabolic acidosis in your differential diagnosis.
Management
When managing a patient with DKA, first consider how sick the patient is and whether they are in the right environment. Go back to basics and think about “oxygen, intravenous (IV) fluids, monitors.” These patients should have a monitored bed and 2 IVs in place for resuscitation. They may also require an arterial or central line for frequent bloodwork (blood testing). In general, you will need to get blood glucose levels every 1 or 2 hours, and you will need to get electrolytes, blood gases, and a bicarbonate level every 4 hours. It is a good idea to have a flow sheet for tracking purposes.
When first speaking to the emergency physician about the patient, there are important questions to ask: How much fluid have they started? Has insulin been started and at what rate? Have they given any supplemental potassium yet?
Regarding where to admit the patient, they will need a step-down bed (ie, a location with closer monitoring including the ability to monitor arterial lines due to a lower nurse-to-patient ratio than a standard ward bed) at minimum because of the frequency of bloodwork required. You should be considering intensive care unit (ICU)-level care for a patient with refractory hypotension, pH <7.0, or altered mental status. These patients would fall into the “severe DKA” category. However, we often monitor their initial response to fluids and insulin therapy in the emergency department (ED) to see if they are making improvements. If they are, this means they would be appropriate for a step-down bed.
In order of most urgent to least urgent, the issues you will have to manage are hemodynamic instability, electrolyte abnormalities, anion gap metabolic acidosis, hyperglycemia, and identification and treatment of the precipitating cause.
1. Hemodynamic instability: When a patient presents with DKA, they already have a volume deficit of several liters. First they need IV fluid (normal saline [NS] or Ringer lactate) boluses to correct this volume depletion. A reasonable management strategy is to start with 1 to 2 L of IV boluses, followed by 500 mL/h for 4 hours, then 250 mL/h and reassess. Be more cautious in patients with underlying congestive heart failure or renal failure. Watch fluid balance and urine output carefully.
2. Electrolyte abnormalities: The primary issue here is total body potassium deficit (see Hypokalemia). At first, the potassium may appear elevated due to the shift out of cells in metabolic acidosis. However, once the acidosis improves, the potassium levels will swiftly drop. This will be exacerbated by insulin therapy. Therefore, it is important to be proactive to ensure that the potassium levels stay in the normal range. For example, even with potassium up to 5.0 mmol/L, you may be adding potassium into the IV fluids. You may also need to supplement potassium orally every 1 to 2 hours.
3. Anion gap metabolic acidosis (AGMA): This will be corrected with IV insulin and fluids. Start at approximately 0.1 IU/kg/h and monitor bloodwork as mentioned previously. If the blood glucose level falls below 15 mmol/L, add dextrose (glucose) to the IV fluid. The goal of the insulin infusion is not to correct the hyperglycemia—the goal is to correct the elevated anion gap metabolic acidosis. One reason to hold the insulin infusion briefly would be if the potassium levels fall below 3.3 mmol/L, which is why it is important to prevent low potassium levels.
4. Hyperglycemia: This will be corrected primarily by IV fluid administration, IV insulin therapy, and treating the precipitating cause. Correcting the hyperglycemia is not the primary purpose of the IV insulin therapy. Plan to keep the glucose levels between 12 mmol/L and 14 mmol/L initially.
5. Identification and treatment of the precipitating cause: One way to remember the precipitating factors of DKA is to remember the 9 I’s: infection, ischemia, infarction, intoxication, insulin nonadherence, inflammation, iatrogenic/drugs, in utero (for pregnancy), and initial presentation of type 1 diabetes mellitus.
Finally, make sure to monitor how quickly you are correcting the serum osmolality and the serum glucose. Cerebral edema can occur if you correct too quickly, so monitor the sodium and glucose levels closely.
In severe DKA with a pH <6.9, you can consider administering IV bicarbonate as well, with a goal to get a pH >7.0.
When can you switch the patient over to subcutaneous insulin? When the anion gap has normalized with low insulin requirements (<2 IU/h), the glucose level is <15 mmol/L, and the patient can tolerate oral intake. Give the first dose of subcutaneous fast-acting insulin 1 to 2 hours prior to discontinuing the IV insulin to allow for overlap.
Finally, always remember that if you are unsure or uncomfortable, please ask for help from the on-call senior medical resident (SMR) or internist.
Credits
I’d like to say thank you to my coauthors: Doctor Roman Jaeschke (Divisions of Critical Care and Internal Medicine; editor for this video) and Doctor Ally Prebtani (Divisions of Internal Medicine and Endocrinology; consultant for this video).
References used to create this Rapid are listed above and include the McMaster Textbook of Internal Medicine, The Intern at Work podcasts and infographics, and 2018 clinical practice guidelines by Diabetes Canada.
Thank you for watching this Rapid Refresher on DKA.
 English
English
 Español
Español
 українська
українська