Internal Medicine Rapid Refreshers is a series of concise information-packed videos refreshing your knowledge on key medical issues that general practitioners may encounter in their daily practice. This episode guides you through the management of asthma exacerbations.
Contents
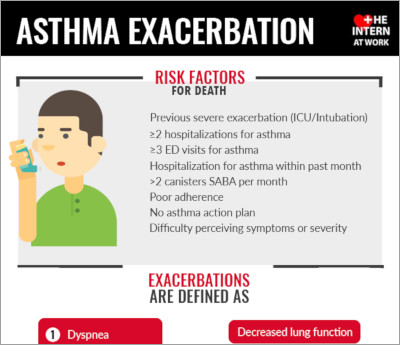
Infographic
Click to view the full image.
Infographic courtesy of The Intern at Work (theinternatwork.com).
Useful links
- Chapter on asthma from the McMaster Textbook of Internal Medicine
- Podcast on asthma exacerbation from The Intern at Work
Transcript
Introduction
I’m Siobhan Deshauer, a senior medical resident at McMaster University. In this video we will be going through a practical approach to the diagnosis and management of an acute asthma exacerbation. This video is intended for practitioners who are returning to general internal medicine during the coronavirus disease 2019 (COVID-19) pandemic. Always remember that there are physicians in the hospital and at home that you can reach out to at any time if you need further assistance.
Overview
Asthma is characterized by cough, wheezing, shortness of breath, and chest tightness, with variable expiratory airflow obstruction.
Some common triggers for the symptoms include a viral or bacterial infection, environmental triggers like an allergen or smoke, exercise, medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or beta-blockers, and medication nonadherence.
Other important mimickers that can seem like asthma include a pneumothorax, anaphylaxis, and a pulmonary embolism.
Investigations
Initial investigations are aimed at diagnosing the trigger, excluding other causes, and determining the severity of the asthma exacerbation.
Begin with the basic bloodwork (blood testing): complete blood count (CBC), electrolytes, and blood gas. Pay special attention to the partial pressure of carbon dioxide (pCO2) level in the blood gas analysis. In an asthma exacerbation we expect the CO2 level to be lower than normal due to hyperventilation. If it is elevated or even normal, this is concerning for respiratory muscles tiring and the patient needs to be monitored closely for the need for intubation.
Order a chest x-ray to look for infiltrates or a pneumothorax; an electrocardiography (ECG) to rule out ischemia or right heart strain; and infectious work-up, including a nasopharyngeal swab and sputum culture. If the patient is not bringing up sputum on their own, do not order a sputum induction during the COVID-19 pandemic, as this risks aerosolizing the virus.
If possible, order spirometry. This is helpful because a forced expiratory volume in 1 second (FEV1) <50% of the predicted value indicates a severe asthma exacerbation.
Acute management
The acute management includes 3 main therapies: oxygen, bronchodilators, and corticosteroids. A severe asthma exacerbation may also require magnesium sulfate and ventilatory support. Clinical signs of a severe exacerbation include a heart rate >120 beats/min, respiratory rate >30 breaths/min, and the use of accessory muscles on inspiration.
Start with the basics: Make sure the patient is in a monitored setting with 2 intravenous (IV) lines and oxygen available. Oxygen should be applied to maintain an oxygen saturation >92%.
Then give short-acting bronchodilators: salbutamol (brand name Ventolin) and ipratropium bromide (brand name Atrovent). Both medications should be dosed at 4 to 8 puffs every 15 minutes for a total of 3 treatments. Then reassess the patient. If symptoms are improving, give salbutamol and ipratropium at 2 to 4 puffs every 4 hours and an additional salbutamol 1 to 2 puffs every 1 hour as needed.
All patients should receive corticosteroids. For a mild exacerbation, give prednisone 40 to 60 mg daily for 5 to 7 days. For a severe exacerbation, give methylprednisolone 125 mg IV and switch to oral prednisone when the patient is stable.
Magnesium sulfate should be considered for severe cases that are not responding to initial treatments. Give 2 g IV over 20 minutes. Be sure the patient is on a cardiac monitor, as magnesium sulfate can cause hypotension and bradycardia. These patients need to be monitored closely, especially in the first few hours.
Call the intensive care unit (ICU) if you see signs of respiratory failure or if the CO2 continues to rise despite treatment. Do not initiate bilevel positive airway pressure (BiPAP) therapy during the COVID-19 pandemic, as this is an aerosolizing procedure. Instead, discuss intubation with the ICU attending physician.
Summary and references
In summary, when treating an asthma exacerbation be sure the patient is in a monitored setting and treat them with oxygen, bronchodilators, and corticosteroids. For a severe exacerbation try magnesium sulfate. Be sure to watch the pCO2 level closely, remembering that an elevated or even normal pCO2 level may be a sign of tiring of the respiratory muscles.
For more information, see the chapter in the McMaster Textbook of Internal Medicine on asthma and the infographic from The Intern at Work (both linked above)
Thank you to those who collaborated on this video, including respirologist Doctor Paul O’Byrne (Division of Respirology).
 English
English
 Español
Español
 українська
українська