Glikson M, Nielsen JC, Kronborg MB, et al; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021 Sep 14;42(35):3427-3520. doi: 10.1093/eurheartj/ehab364. Erratum in: Eur Heart J. 2022 Feb 16;: PMID: 34455430.
Writing Committee Members, Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2019 Sep;16(9):e128-e226. doi: 10.1016/j.hrthm.2018.10.037. Epub 2018 Nov 6. PMID: 30412778.
Definition, Etiology, PathogenesisTop
Intraventricular blocks may be of a His bundle branch block pattern, a fascicular block pattern, or both and result from significant slowing or interruption of conduction. Possible patterns of intraventricular block include:
1) Left anterior or posterior fascicular block.
2) Right bundle branch block (RBBB) (Figure 3.2-5) or left bundle branch block (LBBB) (Figure 3.2-6).
3) RBBB with left anterior or posterior fascicular block (bifascicular block; according to the definition by the European Society of Cardiology, isolated LBBB is also a bifascicular block).
Trifascicular block refers to simultaneous or alternate conduction impairment in all fascicles. This term is also sometimes used in the case of a bifascicular block with first-degree atrioventricular (AV) block, but the definition is not accurate, as PR prolongation in such patients could be related to the AV node and not to a block in the remaining fascicle. Simultaneous impairment in all 3 fascicles presents as complete heart block.
Causes of RBBB: Congenital heart disease (most commonly atrial septal defect), ischemic heart disease (IHD), degenerative or idiopathic fibrosis. This is frequently an isolated finding with no other morphologic cardiac alterations. Features of a pseudo-RBBB with ST-segment elevation are observed in Brugada syndrome.
Causes of LBBB: Structural heart disease: IHD, cardiomyopathy (particularly dilated cardiomyopathy), myocarditis, congenital or acquired heart disease, connective tissue disease, myocardial infiltrates in the course of various conditions, idiopathic fibrosis, or calcifications. At times this is an isolated finding with no other morphologic cardiac alterations.
Intraventricular blocks may be caused by antiarrhythmic drugs, particularly class I drugs (see Table 3.4-1) and amiodarone.
Clinical Features and Natural HistoryTop
Intraventricular blocks without advanced AV block are usually asymptomatic. In patients with LV dysfunction and heart failure, LBBB can worsen the LV dysfunction and mitral regurgitation.
Patients with bifascicular blocks are at risk of slow progression to advanced or complete AV block (this should be suspected in patients with bifascicular block and new-onset syncope).
DiagnosisTop
Diagnosis is based on electrocardiographic (ECG) criteria.
1. Left fascicular block (Figure 3.2-7):
1) Left axis deviation >−30 degrees (anterior fascicular block) or right axis deviation >+90 degrees (posterior fascicular block).
2) Narrow QRS complex <0.12 seconds.
3) Waves:
a) A dominant S wave in leads II, III, and aVF (inferior leads are predominantly negative), a small Q wave and a dominant R wave in leads I and aVL (lateral leads are predominantly positive): Anterior fascicular block.
b) A dominant S wave in leads I and aVL (lateral leads predominantly negative), a dominant R wave in leads II, III, and aVF (inferior leads are predominantly positive): Posterior fascicular block.
2. Bundle branch block:
1) Wide QRS complex ≥0.12 seconds.
2) ST segments and T waves are usually discordant from the dominant deflection of the QRS complex.
3) QRS pattern:
a) rsR, rSR, or rsr patterns, or rarely a wide-notched R-wave pattern in V1 to V2: RBBB (see Figure 3.2-3). rS in V1: LBBB. In summary: V1: with wide positive QRS, think of RBBB; with wide negative QRS, think of LBBB.
b) Monophasic QRS complexes with a notched or biphasic R wave in V5 to V6: LBBB (see Figure 3.2-3). Rs, RS in V6: RBBB.
TreatmentTop
1. Management of the underlying condition.
2. Indications for pacemaker implantation in patients with bundle branch block:
1) Syncope, bundle branch block, and positive electrophysiologic study findings defined as a His-ventricular (HV) interval ≥70 milliseconds (conduction time below the AV node) or triggering second-degree or third-degree AV block in the His bundle/Purkinje fibers during atrial stimulation with increasing frequency or pharmacologic challenge.
2) Alternate bundle branch block, regardless of symptoms.
3) Pacing may be considered in selected patients with unexplained syncope and bifascicular block without electrophysiologic study (the elderly, frail patients, high risk, recurrent syncope, or all), but it is not recommended for asymptomatic bundle branch block or bifascicular block.
3. Indications for biventricular pacing (cardiac resynchronization therapy): see Chronic Heart Failure.
FiguresTop
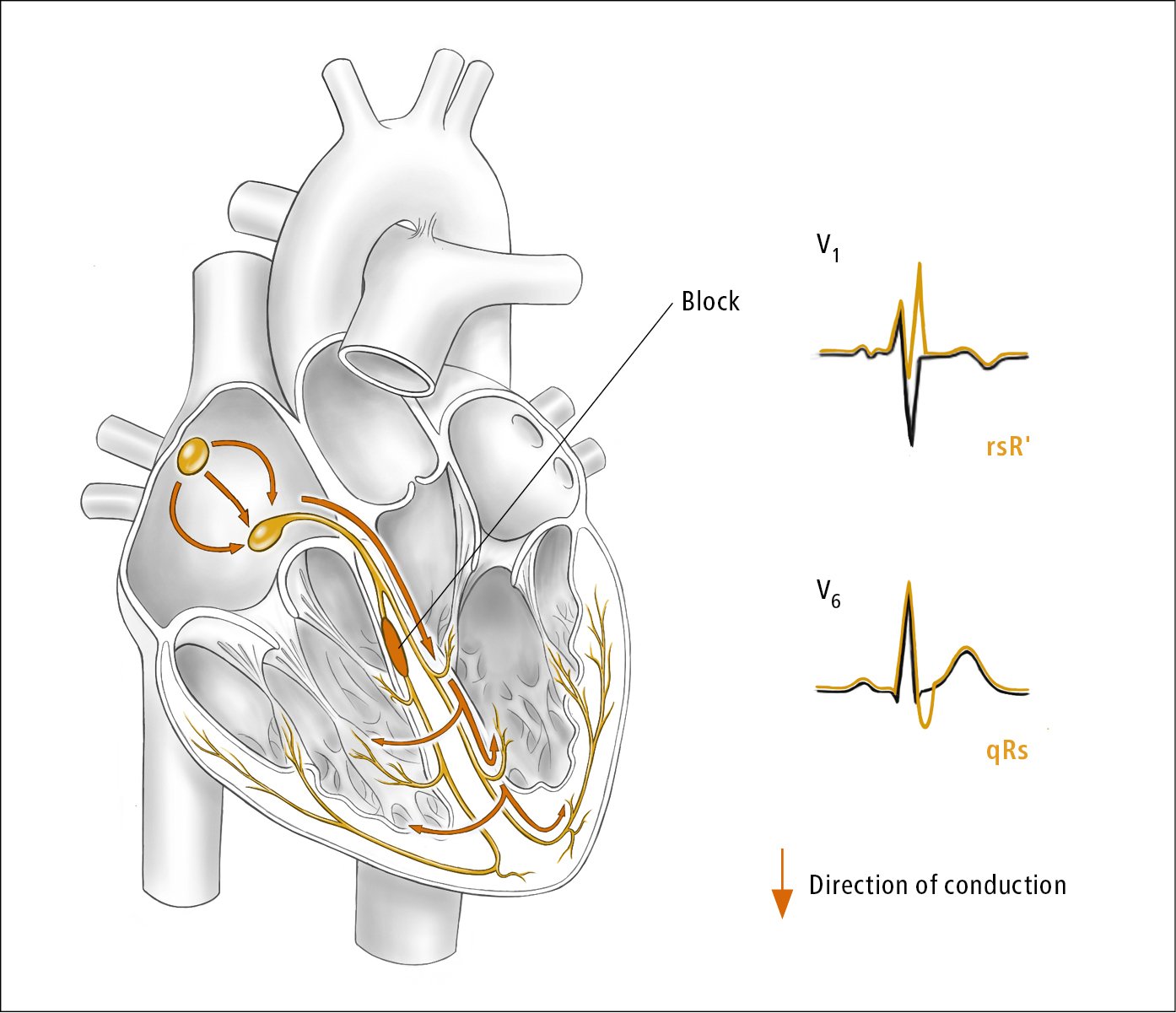
Figure 3.2-5. Right bundle branch block. Illustration courtesy of Dr Shannon Zhang.
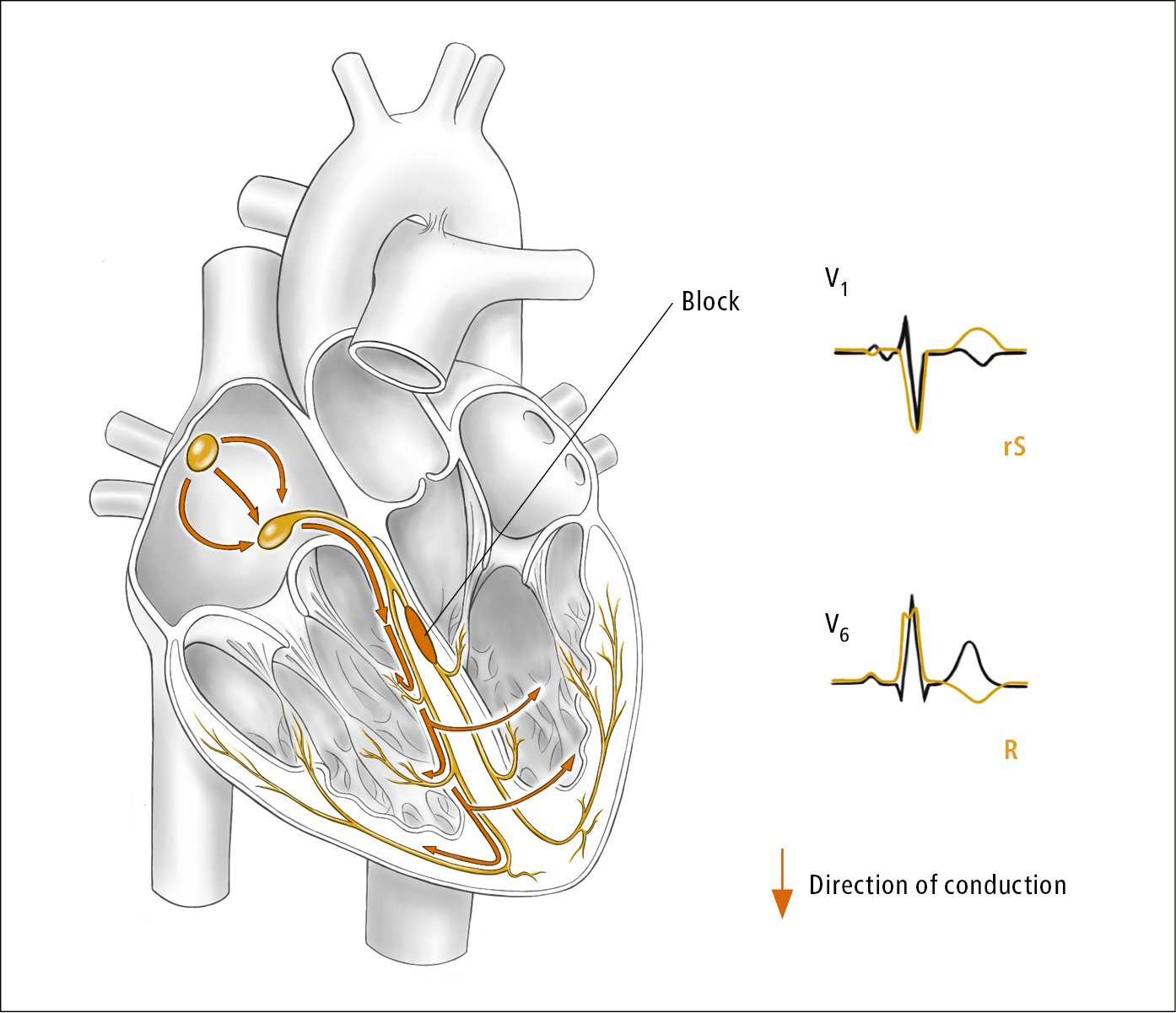
Figure 3.2-6. Left bundle branch block. Illustration courtesy of Dr Shannon Zhang.
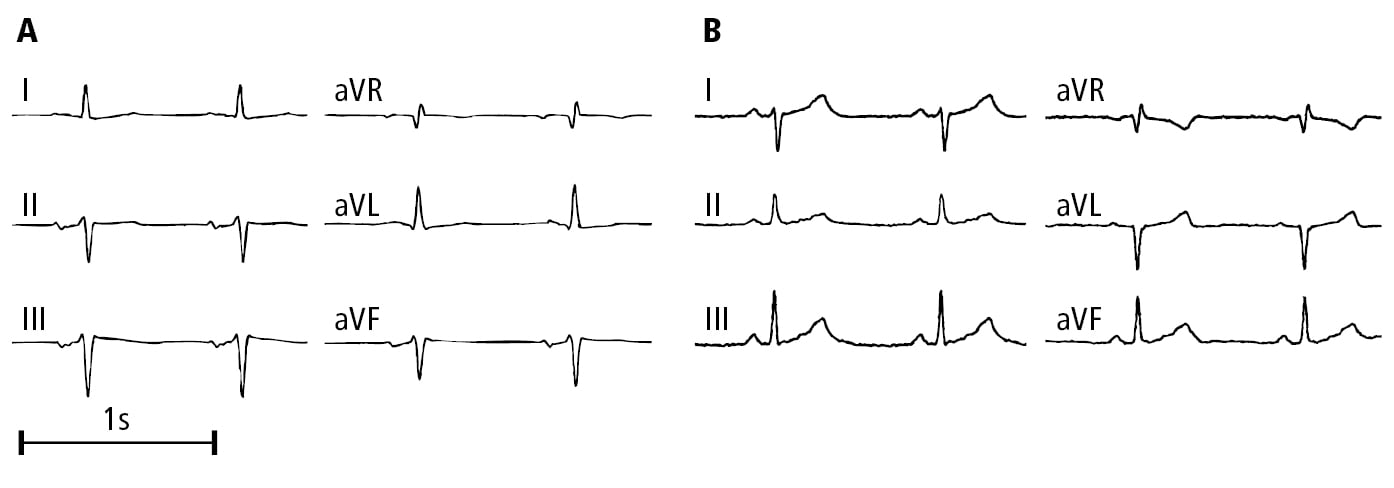
Figure 3.2-7. Electrocardiography (ECG) (limb leads) of patients with left fascicular block: A, left anterior fascicular block; B, left posterior fascicular block. Figure courtesy of Dr Andrzej Stanke.