Siglas y abreviaturas: AASLD — American Association for the Study of Liver Diseases, ACG — American College of Gastroenterology, ACOD — anticoagulantes orales directos, AFP — α-fetoproteína, APTT (activated partial thromboplastin time) — tiempo de tromboplastina parcial activado, AVK — antagonista de la vitamina K, HBPM — heparina de bajo peso molecular, HNF — heparina no fraccionada, RMN — resonancia magnética nuclear, SBC — síndrome de Budd-Chiari, TC — tomografía computarizada, TIPS (transjugular intrahepatic portosystemic shunt) — derivación portosistémica intrahepática transyugular
Introducción
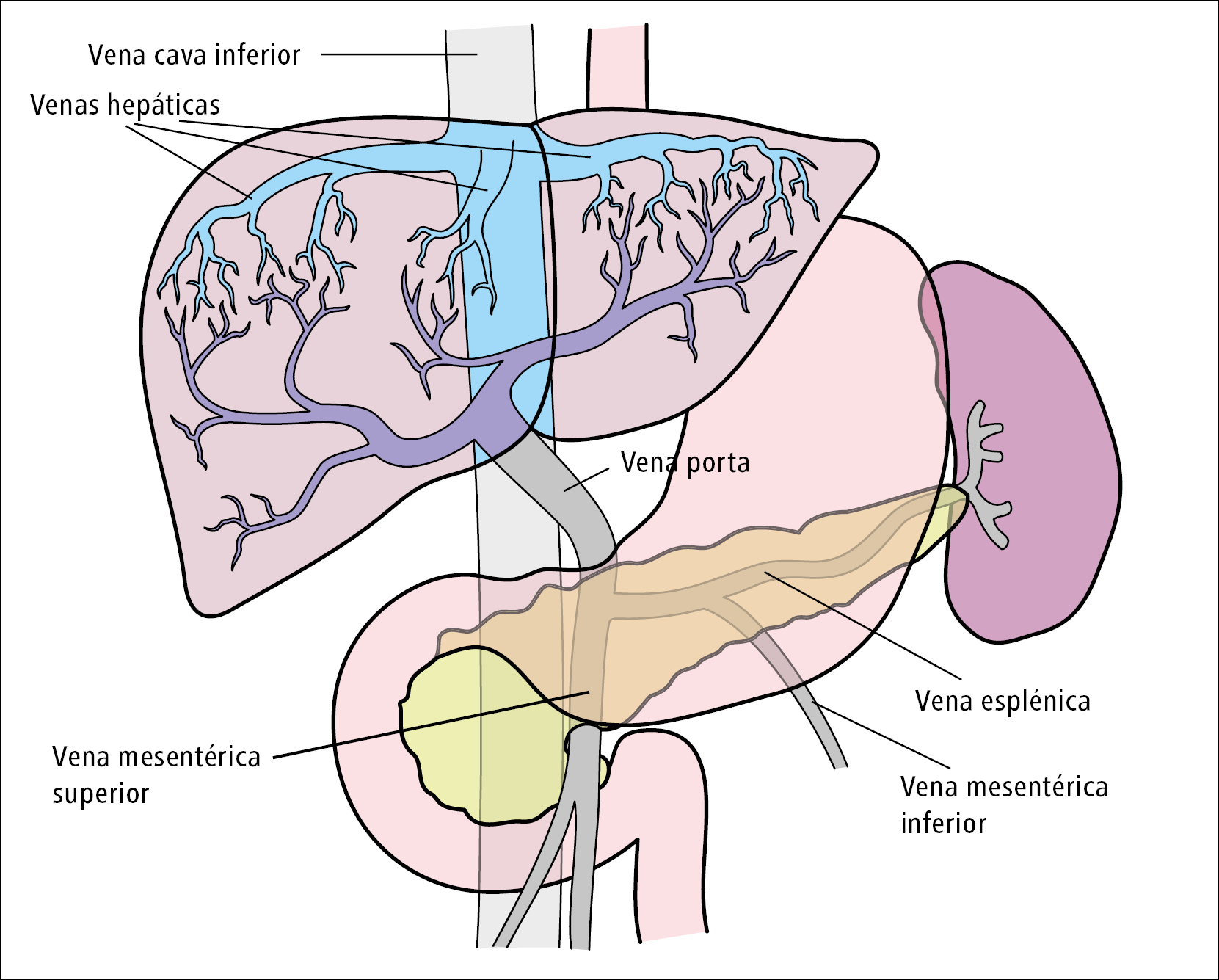
Las enfermedades de la vena porta y las venas hepáticas tienen una importancia clínica considerable, puesto que pueden desembocar en insuficiencia hepática aguda, enfermedad hepática crónica e hipertensión portal, con las complicaciones que esta conlleva. Desgraciadamente, la literatura disponible sobre el manejo de las enfermedades vasculares hepáticas es bastante limitada. En los últimos 2 años, el American College of Gastroenterology (ACG)1 y la American Association for the Study of Liver Diseases (AASLD)2 han publicado documentos sobre las enfermedades vasculares hepáticas y los trastornos de la coagulación en las enfermedades hepáticas. El ACG1 ha elaborado unas guías mediante la metodología GRADE. Las recomendaciones se han clasificado como fuertes [F] o débiles [D], mientras que la calidad de los datos en los que se han basado se ha clasificado en alta [A], moderada [M], baja [B] o muy baja [MB]. Desgraciadamente, la mayoría de las recomendaciones son débiles, con una calidad de datos baja o muy baja. Los expertos de la AASLD han publicado indicaciones de manejo, ya que han considerado que el número de ensayos clínicos aleatorizados (ECA) es insuficiente para elaborar unas guías. En este artículo, redactado a partir de los documentos mencionados del ACG y la AASLD, se presentan las recomendaciones e indicaciones sobre la trombosis de la vena porta y las venas hepáticas (fig. 1).
Figura 1. Esquema del sistema portal y las venas hepáticas
Bibliografía:
1. Simonetto D.A., Singal A.K., Garcia-Tsao G. y cols., ACG Clinical Guideline: Disorders of the hepatic and mesenteric circulation, Am. J. Gastroenterol., 2020; 115: 18-402. Northup P.G., Garcia-Pagan J.C., Garcia-Tsao G. y cols., Vascular liver disorders, portal vein thrombosis, and procedural bleeding in patients with liver disease: 2020 practice guidance by the American Association for the Study of Liver Diseases, Hepatology, 2021; 73: 366-413
3. Yerdel M.A., Gunson B., Mirza D. y cols., Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management, and outcome, Transplantation, 2000; 69: 1873-1881
4. Plessier A., Darwish-Murad S., Hernandez-Guerra M. y cols., Acute portal vein thrombosis unrelated to cirrhosis: a prospective multicenter follow-up study, Hepatology, 2010; 51: 210-218
5. de Franchis R., Baveno V.I.F., Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension, J. Hepatol., 2015; 63: 743-752
6. Hollingshead M., Burke C.T., Mauro M.A. y cols., Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis, J. Vasc. Interv. Radiol., 2005; 16: 651-661
7. Riva N., Ageno W., Poli D. y cols., Safety of vitamin K antagonist treatment for splanchnic vein thrombosis: a multicenter cohort study, J. Thromb. Haemost., 2015; 13: 1019-1027
8. European Association for the Study of the Liver, EASL Clinical Practice Guidelines: Vascular diseases of the liver, J. Hepatol., 2016; 64: 179-202
9. Nery F., Valadares D., Morais S. y cols., Efficacy and safety of direct-acting oral anticoagulants use in acute portal vein thrombosis unrelated to cirrhosis, Gastroenterol.Res., 2017; 10: 141-143
10. Naymagon L., Tremblay D., Zubizarreta N. y cols., The efficacy and safety of direct oral anticoagulants in noncirrhotic portal vein thrombosis, Blood Adv., 2020; 4: 655-666
11. Hamulyak E.N., Daams J.G., Leebeek F.W.G. y cols., A systematic review of antithrombotic treatment of venous thromboembolism in patients with myeloproliferative neoplasms, Blood Adv., 2021; 5: 113-121
12. Di Nisio M., Valeriani E., Riva N. y cols., Anticoagulant therapy for splanchnic vein thrombosis: ISTH SSC Subcommittee Control of Anticoagulation, J. Thromb. Haemost., 2020; 18: 1562-1568
13. Undas A., Zawilska K., Inhibitory czynnika Xa (fondaparynuks, rywaroksaban, apiksaban, edoksaban), https://www.mp.pl/interna/chapter/B16.II.2.34.2 (acceso: 6.01.2022)
14. Nery F., Chevret S., Condat B. y cols., Causes and consequences of portal vein thrombosis in 1,243 patients with cirrhosis: results of a longitudinal study, Hepatology, 2015; 61: 660-667
15. Bianchini M., Cavani G., Bonaccorso A. y cols., Low molecular weight heparin does not increase bleeding and mortality post-endoscopic variceal band ligation in cirrhotic patients, Liver Int., 2018; 38: 1253-1262
16. Kuetting D., Wolter K., Luetkens J. y cols., AngioJet-assisted transvenous-transhepatic mechanical thrombectomy in the portal vein., Pol. J. Radiol., 2018; 83: e536-e44
17. Salem R., Vouche M., Baker T. y cols., Pretransplant portal vein recanalization-transjugular intrahepatic portosystemic shunt in patients with complete obliterative portal vein thrombosis, Transplantation, 2015; 99: 2347-2355
18. Qi X., Guo X., Yoshida E.M. y cols., Transient portal vein thrombosis in liver cirrhosis, BMC Med., 2018; 16: 83
19. Senzolo M., Sartori M.S., Rossetto V. y cols., Prospective evaluation of anticoagulation and transjugular intrahepatic portosystemic shunt for the management of portal vein thrombosis in cirrhosis, Liver Int., 2012; 32: 919-927
20. Northup P., Reutemann B., Management of coagulation and anticoagulation in liver transplantation candidates, Liver Transpl., 2018; 24: 1119-1132
21. Loffredo L., Pastori D., Farcomeni A., Violi F., Effects of anticoagulants in patients with cirrhosis and portal vein thrombosis: a systematic review and meta-analysis, Gastroenterology, 2017; 153: 480-487
22. Lee H.F., Chan Y.H., Chang S.H. y cols., Effectiveness and safety of non-vitamin K antagonist oral anticoagulant and warfarin in cirrhotic patients with nonvalvular atrial fibrillation, J. Am. Heart Assoc,. 2019; 8: e011 112
23. De Gottardi A., Trebicka J., Klinger C. y cols., Antithrombotic treatment with direct-acting oral anticoagulants in patients with splanchnic vein thrombosis and cirrhosis, Liver Int., 2017; 37: 694-699
24. Intagliata N.M., Maitland H., Pellitier S., Caldwell S.H., Reversal of direct oral anticoagulants for liver transplantation in cirrhosis: A step forward, Liver Transpl., 2017; 23: 396-397
25. Faraoun S.A., Boudjella Mel A., Debzi N. y cols., Budd-Chiari syndrome: a prospective analysis of hepatic vein obstruction on ultrasonography, multidetector-row computed tomography and MR imaging, Abdom. Imaging., 2015; 40: 1500-1509
26. Van Wettere M., Purcell Y., Bruno O. y cols., Low specificity of washout to diagnose hepatocellular carcinoma in nodules showing arterial hyperenhancement in patients with Budd-Chiari syndrome, J. Hepatol., 2019; 70: 1123-1132
27. Ren W., Qi X., Yang Z. y cols., Prevalence and risk factors of hepatocellular carcinoma in Budd-Chiari syndrome: a systematic review, Eur. J. Gastroenterol. Hepatol., 2013;
28. Moucari R., Rautou P.E., Cazals-Hatem D. y cols., Hepatocellular carcinoma in Budd-Chiari syndrome: characteristics and risk factors, Gut, 2008; 57: 828835
29. Pieri L., Paoli C., Arena U. y cols., Safety and efficacy of ruxolitinib in splanchnic vein thrombosis associated with myeloproliferative neoplasms, Am. J. Hematol., 2017; 92: 187-195
30. Sharma S., Texeira A., Texeira P. y cols., Pharmacological thrombolysis in Budd Chiari syndrome: a single centre experience and review of the literature, J. Hepatol., 2004; 40: 172-180
31. Perello A., Garcia-Paga n J.C., Gilabert R. y cols., TIPS is a useful long-term derivative therapy for patients with Budd-Chiari syndrome uncontrolled by medical therapy, Hepatology, 2002; 35: 132-139c
32. Oldakowska-Jedynak U., Ziarkiewicz M., Ziarkiewicz-Wroblewska B. y cols., Myeloproliferative neoplasms and recurrent thrombotic events in patients undergoing liver transplantation for Budd-Chiari syndrome: a single-center experience, Ann.Transplant., 2014; 19: 591–597
 Español
Español
 English
English
 українська
українська