Panchal AR, Berg KM, Hirsch KG, et al. 2019 American Heart Association Focused Update on Advanced Cardiovascular Life Support: Use of Advanced Airways, Vasopressors, and Extracorporeal Cardiopulmonary Resuscitation During Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2019 Dec 10;140(24):e881-e894. doi: 10.1161/CIR.0000000000000732. Epub 2019 Nov 14. PMID: 31722552.
Panchal AR, Berg KM, Kudenchuk PJ, et al. 2018 American Heart Association Focused Update on Advanced Cardiovascular Life Support Use of Antiarrhythmic Drugs During and Immediately After Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2018 Dec 4;138(23):e740-e749. doi: 10.1161/CIR.0000000000000613. PMID: 30571262; PMCID: PMC7324904.
Duff JP, Topjian A, Berg MD, Chan M, Haskell SE, Joyner BL Jr, Lasa JJ, Ley SJ, Raymond TT, Sutton RM, Hazinski MF, Atkins DL. 2018 American Heart Association Focused Update on Pediatric Advanced Life Support: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2018 Dec 4;138(23):e731-e739. doi: 10.1161/CIR.0000000000000612. PMID: 30571264.
Wong GC, van Diepen S, Ainsworth C, et al; CCS Post Cardiac Arrest Guidelines Committee. Canadian Cardiovascular Society/Canadian Cardiovascular Critical Care Society/Canadian Association of Interventional Cardiology Position Statement on the Optimal Care of the Postarrest Patient. Can J Cardiol. 2017 Jan;33(1):1-16. doi: 10.1016/j.cjca.2016.10.021. Epub 2016 Nov 3. Review. PubMed PMID: 28024548.
Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015 Nov 3;132(18 Suppl 2):S444-64. doi: 10.1161/CIR.0000000000000261. Review. Erratum in: Circulation. 2015 Dec 15;132(24):e385. PubMed PMID: 26472995.
Monsieurs KG, Nolan JP, Bossaert LL, et al; ERC Guidelines 2015 Writing Group. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation. 2015 Oct;95:1-80. doi: 10.1016/j.resuscitation.2015.07.038. Epub 2015 Oct 15. PubMed PMID: 26477410.
Definition, etiology, pathogenesisTop
Cardiac arrest refers to cessation of cardiac mechanical function characterized by the absence of palpable pulse, lack of response to stimulation, and apnea or agonal respirations. If not rapidly reversed, cardiac arrest progresses to death.
Primary cardiac arrest is caused by or associated with a principal cardiac condition, such as:
1) Coronary artery disease (eg, acute coronary syndrome [ACS]/ischemic heart disease, coronary vasospasm, spontaneous coronary artery dissection).
2) Cardiomyopathies (eg, ischemic cardiomyopathy, nonischemic dilated cardiomyopathy, hypertrophic cardiomyopathy, infiltrative disorders such as amyloidosis or sarcoidosis, arrhythmogenic right ventricular cardiomyopathy, ventricular noncompaction, myocarditis).
3) Congenital arrhythmogenic heart diseases (eg, long QT syndrome, short QT syndrome, Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia, idiopathic ventricular fibrillation).
4) Structural heart disease (eg, severe aortic stenosis, mitral valve prolapse, anomalous coronary artery circulation, Wolff-Parkinson-White syndrome, sinus node disturbances, atrioventricular conduction disturbances).
5) Other (eg, cardiac tamponade, commotio cordis, aortic dissection).
Secondary cardiac arrest occurs due to noncardiac causes, such as pulmonary embolism, respiratory arrest, multisystem trauma, hemorrhage, acute intracerebral hemorrhage, intoxication, seizures, or near-drowning.
Rhythms in cardiac arrest:
1) Ventricular fibrillation (VF) (Figure 3.3-1).
2) Pulseless ventricular tachycardia (pVT) or ventricular flutter.
3) Asystole: Lack of electrical and mechanical activity of the heart (also diagnosed at a heart rate <10 beats/min).
4) Pulseless electrical activity (PEA): Lack of a hemodynamically effective mechanical contraction of the heart despite preserved organized electrical activity.
Asystole and PEA commonly result from secondary cardiac arrest or more prolonged primary cardiac arrest (degenerated from VF or pVT) and therefore always require a search for reversible causes.
ManagementTop
Basic life support (BLS): Figure 3.3-2.
Cardiopulmonary resuscitation (CPR) refers to interventions (chest compressions and ventilation) aimed at maintaining circulation and oxygenation of blood in an individual with cardiac arrest. High-quality CPR is essential to improving survival rates. The steps described below refer to nontraumatic cardiac arrest in adults when help is provided by a health care professional.
If the patient is not in a hospital bed (eg, on the floor), do not delay care to move the patient onto a stretcher, provided the location is safe and permits compressions. Survival from cardiac arrest decreases by up to 10% per minute that defibrillation is delayed in the absence of CPR. Begin CPR where the patient is (as long as it is safe) and bring the defibrillator to the patient.
1. Make sure the patient and you (as well as other rescuers) are safe. Control possible hazards (as necessary, call the police, fire department, or other emergency agency for additional assistance).
2. Assess the patient’s consciousness. If the patient does not respond to voice and gentle shaking, assume that they are unconscious.
3. Shout or phone for help.
4. Clear/open the airway (Figure 3.3-3). Place the unconscious patient on their back. Then tilt the head backwards (this maneuver is contraindicated in individuals with suspected cervical spine injury) and examine the mouth, removing any visible foreign bodies. Proceed to chin lift or jaw thrust; these two maneuvers may be performed in patients with suspected cervical spine injury, provided that the head is stabilized in a neutral position without tilting.
5. Assess respirations. Look for chest movements, listen at the patient’s mouth for the sounds of inspiration and expiration, place your cheek near the patient’s mouth to feel for air movement, and check for pulse at the carotid (or femoral) artery for a maximum of 10 seconds. Do not delay compressions to check other pulse sites such as the other carotid artery or femoral pulse. If the patient is unresponsive, apneic, and you do not clearly detect a carotid pulse, begin compressions. The lack of chest movements, respiratory sounds, and perceptible air movement indicates apnea, which may be caused by a primary cardiac arrest or by complete airway obstruction, respiratory depression, or respiratory diseases. Agonal respirations (residual single sighs) are treated as apnea. Other sounds accompanying respiration may indicate partial obstruction of the respiratory tract: (1) gurgling due to liquid or semiliquid content in the airways (ie, vomit, blood, respiratory tract secretions); (2) snoring due a partial closure of the throat by the tongue, palate, or foreign body; (3) stridor due to obstruction or swelling at the level of the glottis.
In some cases it may be necessary to clear/open the airway. If the patient is breathing spontaneously, place them in the recovery position (Figure 3.3-4). If a pulse is definitely present in a patient who is not breathing spontaneously, deliver ventilations at the rate of 10 breaths/min without chest compressions (see below). Every 2 minutes check the pulse and look for signs of circulation (ie, spontaneous movements, coughing, breathing). Absence of signs of circulation and of carotid pulse indicate cardiac arrest and require immediate CPR. During CPR check for signs of circulation and pulse every 2 minutes.
6. Call for help. If you are alone, immediately upon discovering apnea, grossly abnormal breathing, or lack of pulse call for expert assistance if at all practical, even if you have to briefly leave the patient for this purpose. When away from the hospital, call local emergency services. Hospitals should have an emergency extension or phone number known to and available for all employees. Exception: in the case of children and infants, before calling for help proceed with CPR for ~1 minute (perform 5 rescue breaths, then 15 sternal compressions, then another 2 breaths and 15 compressions).
7. Start chest compressions. Place the patient in the supine position on a hard surface and compress the center of the sternum. In adults compress from 5 to 6 cm deep at a rate of 100 to 120 compressions/min (~2 compressions/s). In children compress the sternum with one hand, and in infants compress with 2 fingers to one-third the depth of the sagittal dimension of the chest (or 4 cm deep for infants and 5 cm deep for children). To perform compressions in adults, place the heel of one hand in the center of the patient’s chest and the heel of your other hand on the top of the first hand, interlock the fingers of your hands, and keep your arms straight and your shoulders directly over the patient’s chest, all without leaning on the patient’s ribs. Completely release the pressure without taking your hands off the chest; the duration of compression and release should be identical. In adults start with 30 chest compressions followed by 2 rescue breaths, then continue with chest compressions and rescue breaths, maintaining a ratio of 30:2 in nonintubated adult patients. In pediatric patients the optimum ratio of compressions to respirations is not clear, but the American Heart Association (AHA) guidelines propose 30:2 for a single rescuer and 15:2 when the second rescuer is available as reasonable suggestions.
8. Continue ventilation, giving mouth-to-mouth rescue breaths while pinching the patient’s nose if more than one responder is available. In infants perform mouth-to-mouth-and-nose rescue breaths. A lone rescuer should focus on compressions and should avoid excessive interruptions of chest compressions to provide rescue breaths. One breath should last ~1 second (2 rescue breaths [inspiration plus expiration] should last <5 seconds). Make sure the chest rises during inspiration and allow for its complete fall during exhalation. Chest compressions should not be interrupted for >10 seconds while rescue breaths are being delivered. If the rescue breaths are ineffective (ie, the chest does not rise), change the position of the head and jaw and repeat a maximum of 2 ventilation attempts.
9. Defibrillate using an automated external defibrillator (AED). Use an AED immediately when available. Defibrillation of a shockable rhythm within 3 to 5 minutes of a cardiac arrest can increase survival rates by up to 50% to 70%. For each minute that defibrillation is delayed, the likelihood of survival to hospital discharge is reduced by 10% to 12%. Switch on the AED and attach the pads to the chest (one below the right clavicle along the sternum and the other below and to the left of the left nipple in the midaxillary line: Figure 3.3-5). Keep away from the patient for the time the AED is assessing the rhythm and when the shock is being delivered. Charge the AED and trigger the shock whenever indicated by the AED. After 1 defibrillation immediately start CPR and continue for 2 minutes before the AED reevaluates the heart rhythm.
Advanced Life Support or Advanced Cardiac Life Support
Advanced life support (ALS) or advanced cardiac life support (ACLS): Figure 3.3-6.
ALS or ACLS refers to procedures performed by a team of appropriately trained and equipped professional rescuers that are aimed at restoring spontaneous circulation using CPR, advanced airway management (eg, endotracheal intubation, laryngeal mask), defibrillation/cardioversion, and administration of medications.
1. Safety assessment (removal of threats) and diagnosis of cardiac arrest: see Basic Life Support, above.
2. Perform CPR: Figure 3.3-2. Minimize the time necessary for other activities (intubation performed as quickly as possible, preferably <10 seconds; defibrillation <5 seconds; continue CPR while charging the defibrillator [see below]). If possible, the rescuers performing chest compressions should change every 2 minutes.
3. Assess the mechanism of cardiac arrest and defibrillate when indicated. If a defibrillator is immediately available and ready for discharge and cardiac arrest occurred in the presence of rescuers or in the hospital, defibrillation may be attempted before starting CPR. Connect a manual defibrillator and monitor the patient for arrhythmia eligible for defibrillation (VF or pVT). After turning on the defibrillator, make sure that the lead selector is appropriately set to either paddles or standard electrodes (leads I, II, III). Then attach the 3 electrodes to the chest and connect them to the defibrillator (North American electrode placement: white on the right, red on the left lower chest, and black on the left upper chest; European electrode placement: red on the right shoulder, yellow on the left shoulder, green on the left midaxillary line at the costal margin). In the event of asystole on the monitor, check the defibrillator connections (monitor), settings of the signal amplification (gain), and readings from another lead. If in doubt whether the patient is in asystole or low-voltage VF, do not defibrillate and continue CPR. During CPR reassess the heart rhythm every 2 minutes.
Defibrillation using a manual defibrillator:
1) Apply gel (or, more often, defibrillation pads) on the skin of the chest where the paddles are to be placed or on the paddles themselves (self-adhesive defibrillation pads require no gel). Self-adhesive defibrillation pads have several advantages over manual paddles and should be used preferentially when available.
2) Most commonly adhesive pads are placed in the sternal-apical position, as in manual paddles. Depending on the patient’s anatomy and other cardiac arrest features, other acceptable pad positions include (a) bilateral lateral chest walls (biaxillary); (b) one pad at the standard apical position and the other on the right upper back; (c) one pad anteriorly over the left precordium and the other posteriorly just inferior to the left scapula. If adhesive pads are not available and paddles are used, apply the paddles to the chest with a force of ~10 kg (one below the right clavicle along the sternum and the other below and to the left of the left nipple: Figure 3.3-5).
3) Assess the rhythm on the defibrillator monitor (after applying the paddles or adhesive pads temporarily stop CPR). The indication for delivering a shock is VF or pVT. Resume CPR while the defibrillator charges (remove the paddles from the chest for that time).
4) Set the shock energy:
a) Adults: When using biphasic defibrillators, providers should use the manufacturer’s recommended energy dose (ie, initial energy of 120-200 J). If the dose range is unknown, the provider may use a maximal dose of 200 J. The first shock is usually 150 J. The energy of subsequent shocks may be increased to a maximum of 200 J. In monophasic defibrillators the first and subsequent shocks are 360 J.
b) Children: 2 J/kg for the first shock, then increase the charge by 2 J/kg for each subsequent shock (2-4-6-8) to a maximum of 10 J/kg or adult defibrillation charge, whichever is less.
5) Charge the defibrillator (press “charge”).
6) Order all rescuers to move away and stay clear of the patient. Make sure no one is touching either the patient or any objects that are in contact with the patient. At this point stop CPR. If you are using paddles, place them back in the areas of the chest previously covered with gel.
7) Deliver the shock (press and hold the “discharge” or “shock” button).
After delivering the shock, immediately restart CPR for 2 minutes; stop if signs of circulation appear (coughing, breathing, movements). Then reassess the rhythm and if the first shock has not been effective, deliver subsequent shocks every 2 minutes for shockable rhythms. Continue CPR between shocks. Next, establish vascular access (IV or intraosseous), intubate the patient when possible (if not done already), and administer medications (Figure 3.3-6). Tracheal intubation should not delay defibrillation attempts and may be deferred until return of spontaneous circulation (ROSC) is achieved. A series of 3 shocks at intervals <2 minutes may be used in the case of a cardiac arrest occurring during cardiac catheterization or shortly after a surgical cardiac procedure, or in the case of a witnessed cardiac arrest in a patient already connected to a manual defibrillator. Following the first 2 (AHA guidelines) or 3 (European Resuscitation Council [ERC] guidelines) ineffective shocks, administer IV epinephrine 1 mg (10 microg/kg for children). New evidence in out-of-hospital cardiac arrest patients shows increased survival with the use of epinephrine but no difference in neurologically favorable outcome; current guidelines still endorse the use of epinephrine in these patients based on the totality of evidence.Evidence 1Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to the risk of bias and indirectness. Perkins GD, Ji C, Deakin CD, et al; PARAMEDIC2 Collaborators. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2018 Aug 23;379(8):711-721. doi: 10.1056/NEJMoa1806842. Epub 2018 Jul 18. PMID: 30021076. After 3 ineffective shocks, administer IV amiodarone 300 mg (5 mg/kg for children; maximum, 300 mg; see Other Interventions and Tasks, below) before delivering the fourth shock (AHA guidelines). Do not stop CPR for the time the drugs are being administered. If the fourth shock is also ineffective, deliver subsequent shocks every 2 minutes and administer epinephrine 1 mg every 3 to 5 minutes. Consider administration of another 150 mg of amiodarone (you may repeat 5 mg/kg for children) and look for reversible causes of cardiac arrest (see below). Consider changing the position of the defibrillator paddles to a front-to-back position (Figure 3.3-5) or to the opposite middle axillary lines.
In the case of a witnessed cardiac arrest—in particular during electrocardiography (ECG) monitoring that shows VF or pVT—if a defibrillator ready to trigger off a discharge is not immediately available, you may hit the precordial area (sternum) with a clenched fist, delivering a precordial blow or “thump.” This is an attempt to defibrillate with low energy, which is sometimes effective within 30 seconds of the onset of VF or pVT. However, the precordial thump should not delay CPR and defibrillation.
In the case of cardiac arrest with refractory VF or ventricular tachycardia (VT), evidence suggests that a vector change of the defibrillation pads or performing dual sequential external defibrillation may result in more patients attaining ROSC and surviving to hospital discharge (see figure in doi:10.1056/NEJMoa2207304).Evidence 2Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to the risk of bias, imprecision, and generalizability. Cheskes S, Verbeek PR, Drennan IR, et al. Defibrillation Strategies for Refractory Ventricular Fibrillation. N Engl J Med. 2022 Nov 24;387(21):1947-1956. doi: 10.1056/NEJMoa2207304. Epub 2022 Nov 6. PMID: 36342151.
1. Clear/open the airway. Perform endotracheal intubation if the provider is sufficiently skilled in this procedure (this should be completed within 10 seconds). CPR and prompt defibrillation have priority over intubation. If endotracheal intubation is unsuccessful, you may try a laryngeal mask or laryngeal tube. Alternatively, insert an oropharyngeal or nasopharyngeal airway. If there is only one advanced provider who is responsible for both managing the cardiac arrest and for intubating, it is more important to manage the arrest, as long as the patient can be ventilated using a bag-valve-mask, rather than trying to do both complex tasks at the same time.
2. Ventilate the patient using a self-inflating bag (with a valve) that is connected to a reservoir bag and high-flow oxygen (>10-15 L/min) to achieve the highest possible inspired concentration of oxygen during CPR (close to 100%). Before intubation (and also when an oropharyngeal or nasopharyngeal airway is used) ventilate the patient using a face mask, delivering 30 chest compressions followed by 2 rescue breaths. After successful intubation ventilate the patient via the endotracheal tube at a rate of ~8 to 10 breaths/min; synchronization with chest compressions is not necessary. Asynchronous CPR may be also attempted once the airway has been secured using supraglottic airway devices. The ventilation volumes are 6 to 7 mL/kg (500-600 mL) over 1 second. If capnography (measurement of the end-expiratory CO2 levels) is available, it can assist in confirming endotracheal intubation and in the assessment of the effectiveness of ventilation, ROSC, and quality of chest compressions.
3. Look for and treat reversible causes of cardiac arrest, particularly in the event of asystole or PEA but also in the case of VF or pVT not responding to defibrillation. Take history from witnesses and perform a quick targeted physical examination and diagnostic tests during CPR. Reversible causes can be remembered by H’s and T’s; if suspected or confirmed, they should be corrected immediately:
1) Hypoxia.
2) Hypovolemia (eg, hemorrhage, diarrhea).
3) Hydrogen ion or acidosis.
4) Hypothermia.
5) Hyperkalemia, hypokalemia, or other severe electrolyte disturbances (see Electrolyte Disturbances). If no history is known but wide-complex bradycardia or asystole is present, it may be reasonable to treat empirically for hyperkalemia.
6) Tamponade (cardiac; see Pericardiocentesis).
8) Thrombosis (see Pulmonary Embolism).
9) Thrombosis (myocardial infarction).
10) Toxins (eg, drug overdose, poisoning).
11) Trauma: If no other cause is identified, conduct rapid body survey for possible undetected trauma causing hypovolemia.
12) In children check for hypoglycemia.
4. Administer medications. After every IV drug administration during CPR, use an additional 20 mL of 0.9% NaCl to flush the IV catheter. In patients without venous access, medications may be delivered via the intraosseous route.
1) Epinephrine. Indications: asystole, PEA, VF, or pVT not responding to the first 2 (AHA) or 3 (ERC) shocks. Dosage: 1 mg IV in 10 mL of 0.9% NaCl (or nondiluted) every 3 to 5 minutes (in children 10 microg/kg).
2) Amiodarone. Indications: VF or VT not responding to the first 3 shocks. Dosage: 300 mg in 20 mL of 5% glucose (dextrose) as an IV bolus (5 mg/kg in children). In case of persistent VF or VT, an additional 150 mg may be administered; then consider 900 mg/d in a continuous IV infusion.
3) Sodium bicarbonate. Indications: hyperkalemia and tricyclic antidepressant overdose. Outside of these indications, routine use of sodium bicarbonate is not recommended. Dosage: 50 mmol (50 mL of 8.4% solution) IV (1-2 mmol/kg for children); repeat as considered necessary according to the clinical condition and serial blood gas measurements.
4) Magnesium sulfate. Indications: torsades de pointes (polymorphic VT with prolonged QT; Figure 3.3-1). Magnesium is not likely to be effective in terminating polymorphic VT with a normal QT interval. Dosage: 1 to 2 g diluted in 10 mL of 5% glucose IV over 1 to 2 minutes (25-50 mg/kg for children); repeat after 10 to 15 minutes if necessary.
5) Calcium chloride. Indications: hyperkalemia, hypocalcemia, and overdose of calcium channel blockers. There are no data supporting beneficial effects of the use of calcium chloride in other causes of cardiac arrest; recent evidence suggests that it may be harmful in out-of-hospital settings in patients with cardiac arrest without an indication for calcium administration.Evidence 3Weak recommendation (downsides likely outweigh benefits, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness. Vallentin MF, Granfeldt A, Meilandt C, et al. Effect of Intravenous or Intraosseous Calcium vs Saline on Return of Spontaneous Circulation in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA. 2021 Dec 14;326(22):2268-2276. doi: 10.1001/jama.2021.20929. PMID: 34847226; PMCID: PMC8634154. Avoid calcium chloride in patients with severe hyperphosphatemia. Dosage: 10 mL of a 10% CaCl2 solution as an IV bolus (0.2 mL/kg for children); repeat as necessary.
6) Fibrinolysis should not be used routinely in cardiac arrest. You may consider fibrinolytic therapy when the arrest was caused by proven or suspected pulmonary embolism in the absence of absolute contraindications (see Pulmonary Embolism). Consider continuation of CPR for 60 to 90 minutes following the administration of a fibrinolytic agent.
7) Other drugs:
a) IV glucose. Indications: hypoglycemia.
b) IV glucagon. Indications: hypoglycemia (1 mg) and overdose of beta-blockers or calcium channel blockers (5-10 mg; 0.05-0.15 mg/kg in children).
c) Antihistamines (H1 and H2 antagonists) and IV glucocorticoids. Indications: anaphylaxis (see Anaphylaxis and Anaphylactic Shock).
d) IV fluids. Indications: hypovolemia, anaphylaxis, or undifferentiated shock (see Shock).
e) Blood products (eg, red blood cells, frozen plasma, platelet concentrates). Indications: hemorrhage (at the same time make attempts to stop the hemorrhage as soon as possible), coagulopathy.
f) Naloxone. Indications: opioid poisoning or overdose (see Acute Opioid Toxicity).
g) Lipid emulsion therapy. Indications: poisonings involving certain lipophilic medications (overdoses of calcium channel blockers, beta-blockers, some tricyclic antidepressants, local anesthetics, and chlorpromazine). Before using lipid emulsion therapy it is recommended to consult a poison control center or toxicologist. Dosage: 20% lipid emulsion (1-1.5 mL/kg bolus followed by a continuous IV infusion at a rate of 0.25-0.5 mL/kg/min). If cardiovascular stability has not been restored after 5 minutes, the 1.5 mL/kg bolus may be repeated a maximum of 2 times.
5. Cardiac pacing: Electrical pacing during cardiac arrest is generally considered ineffective and therefore is not recommended for routine use. Pacing may be considered for recurrent polymorphic VT when precipitated by bradycardia or pauses or early after cardiac surgery in patients with asystole. Pacing can be done via transcutaneous pads or a temporary transvenous wire.
Management After Restoring Spontaneous Circulation
1. Placement of the unconscious patient with preserved spontaneous breathing in the recovery position (this does not apply to intubated patients; Figure 3.3-4) unless there is an immediate history of suspected trauma, particularly spine injury.
2. Prompt transfer to the intensive care unit (ICU) or high acuity bed. The patient should be transported to the hospital by an ambulance with the appropriate CPR equipment and CPR-competent personnel and moved around the hospital when attended by a hospital resuscitation team, ideally with a connected defibrillator, continuous oxygen therapy with a saturation target ≥92%, secured airway (in unconscious patients), and continued ventilation.
3. Hospitalization in the ICU or an equivalent unit for a time deemed necessary, usually ≥24 hours:
1) Continuous monitoring of ECG, pulse oximetry, blood pressure, and urine output, when deemed necessary supplemented by the use of the central line as well as hemodynamic monitoring with an intra-arterial line.
2) Treatment of arrhythmias (eg, ventricular and supraventricular tachycardias, bradycardia), shock, heart failure, ACS, respiratory failure.
3) Determination of the cause of cardiac arrest and further diagnostic workup and treatment:
a) A repeated broader history and physical examination (if the patient cannot provide information on their own, ask the rescuers, witnesses of the cardiac arrest, family, and other persons living with or close to the patient, and use the available medical records).
b) 12-lead ECG, other diagnostic tests of ACS (cardiac troponin and echocardiography, when necessary), and appropriate treatment if the diagnosis of ACS is established (including revascularization and medical therapies).
c) Chest radiography looking for evidence of various conditions as dictated by clinical situation, for example, pneumothorax, pneumonia, atelectases, pericardial or pleural effusion, or venous congestion. Verify the positioning of the endotracheal tube, gastric tube, and IV catheters.
d) Arterial blood gas measurements and treatment of acid-base disturbances and respiratory insufficiency (administer oxygen when necessary to maintain an arterial hemoglobin oxygen saturation of 92%-96%). Hyperoxia (saturation >96%) may be harmful,Evidence 4Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness. Siemieniuk RAC, Chu DK, Kim LH, et al. Oxygen therapy for acutely ill medical patients: a clinical practice guideline. BMJ. 2018 Oct 24;363:k4169. doi: 10.1136/bmj.k4169. PubMed PMID: 30355567. Chu DK, Kim LH, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018 Apr 28;391(10131):1693-1705. doi: 10.1016/S0140-6736(18)30479-3. Epub 2018 Apr 26. Review. PubMed PMID: 29726345. but hypoxia is more immediately dangerous: if you do not have a pulse oximeter or blood gas readings and the patient is cyanotic or unresponsive, it is reasonable to administer 100% oxygen while awaiting oxygen saturation or blood gas measurements.
e) Measurements of serum electrolyte levels and treatment of electrolyte disturbances. Measurements of blood glucose levels (if >10 mmol/L [180 mg/dL], administer continuous IV insulin).
f) Looking for signs of active bleeding (particularly gastrointestinal bleeding; start appropriate prophylaxis), review of the complete blood count (CBC) (look for anemia and transfuse packed red blood cells when necessary).
g) Kidney and liver function tests.
h) Basic coagulation tests.
i) Toxicology tests in the case of suspected poisoning, with appropriate treatment when indicated.
j) Other investigations to assess for the cause of the arrest as dictated by the clinical situation (eg, chest computed tomography [CT] for suspected pulmonary embolism, echocardiography for suspected ACS or pericardial effusion).
4) Consider bronchoscopy to clear the airway in patients with suspected or documented aspiration.
5) Consider imaging studies of the head in unconscious patients and those with neurologic symptoms to assess for intracranial hemorrhage, ischemic stroke, cerebral edema, or other significant intracranial pathology.
6) In patients who remain comatose (Glasgow Coma Scale [GCS] <8 [see Table 1.5-2] or inability to respond to verbal commands) following ROSC after a VF or pVT arrest, it is recommended to initiate targeted temperature management (TTM) to help improve neurologic prognosis, including improved survival with a good neurologic outcome.Evidence 5Strong recommendation (benefits clearly outweigh downsides; right action for all or almost all patients). Moderate Quality of Evidence (moderate confidence that we know true effects of intervention). Quality of Evidence lowered due to some indirectness (no temperature control in the control group) and expected lack of blinding. Dankiewicz J, Cronberg T, Lilja G, et al; TTM2 Trial Investigators. Hypothermia versus Normothermia after Out-of-Hospital Cardiac Arrest. N Engl J Med. 2021 Jun 17;384(24):2283-2294. doi: 10.1056/NEJMoa2100591. PMID: 34133859. Arrich J, Holzer M, Havel C, Müllner M, Herkner H. Hypothermia for neuroprotection in adults after cardiopulmonary resuscitation. Cochrane Database Syst Rev. 2012 Sep 12;(9):CD004128. doi: 10.1002/14651858.CD004128.pub3. Update in: Cochrane Database Syst Rev. 2016;2:CD004128. PMID: 22972067. Vargas M, Servillo G, Sutherasan Y, Rodríguez-González R, Brunetti I, Pelosi P. Effects of in-hospital low targeted temperature after out of hospital cardiac arrest: A systematic review with meta-analysis of randomized clinical trials. Resuscitation. 2015 Jun;91:8-18. doi: 10.1016/j.resuscitation.2015.02.038. Epub 2015 Mar 20. PMID: 25796995. Nielsen N, Wetterslev J, Cronberg T, et al; TTM Trial Investigators. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013 Dec 5;369(23):2197-206. doi: 10.1056/NEJMoa1310519. Epub 2013 Nov 17. PMID: 24237006. Lower level evidence exists for the use of TTM in cardiac arrest survivors of nonshockable rhythms.Evidence 6Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision of subgroup analysis and lack of blinding. Arrich J, Holzer M, Havel C, Müllner M, Herkner H. Hypothermia for neuroprotection in adults after cardiopulmonary resuscitation. Cochrane Database Syst Rev. 2012 Sep 12;9:CD004128. doi: 10.1002/14651858.CD004128.pub3. Review. PubMed PMID: 22972067. European and American guidelines recommend cooling to 32 to 36 degrees Celsius for ≥24 hours. Canadian guidelines recommend 33 to 36 degrees Celsius. However, new robust randomized controlled trial (RCT) evidence in out-of-hospital settings in patients with cardiac arrest supports the use of normothermia and only initiating TTM for temperatures >37.7 degrees Celsius.Evidence 7Moderate Quality of Evidence (moderate confidence that we know true effects of intervention). Quality of Evidence lowered due to imprecision and lack of blinding. Dankiewicz J, Cronberg T, Lilja G, et al; TTM2 Trial Investigators. Hypothermia versus Normothermia after Out-of-Hospital Cardiac Arrest. N Engl J Med. 2021 Jun 17;384(24):2283-2294. doi: 10.1056/NEJMoa2100591. PMID: 34133859. Our own pattern of TTM practice has evolved over the last few years and is currently directed to keep the temperature of cardiac arrest survivors <37 degrees Celsius. Regardless of the TTM threshold chosen, as hyperthermia contributes to worsened neurologic outcome, fever should be aggressively managed after cardiac arrest. Lastly, there is a strong suggestion of no benefits of cooling with a cold saline infusion before arrival at the hospital. TTM is usually accomplished using ice packs or specialized equipment (eg, cooling blankets, cooling suits, or IV cooling devices). If the decision is to reduce body temperature to <36 degrees Celsius, after the cooling period increase it slowly (0.25-0.5 degrees Celsius/h).
FiguresTop
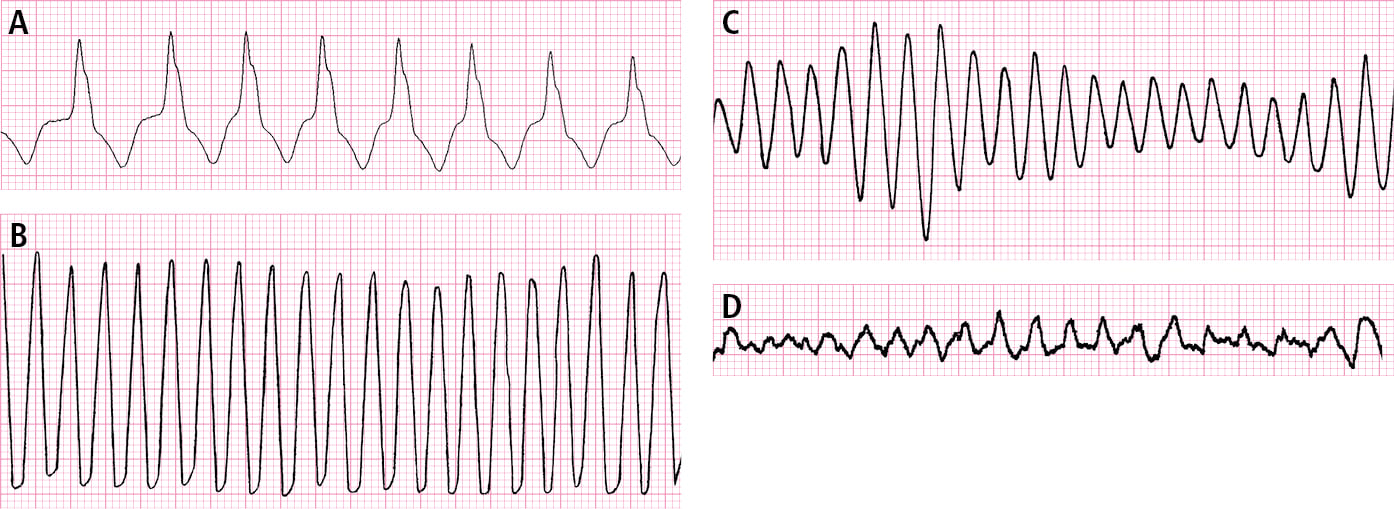
Figure 3.3-1. Ventricular arrhythmia. A, monomorphic ventricular tachycardia. B, ventricular flutter. C, polymorphic ventricular tachycardia. D, ventricular fibrillation.
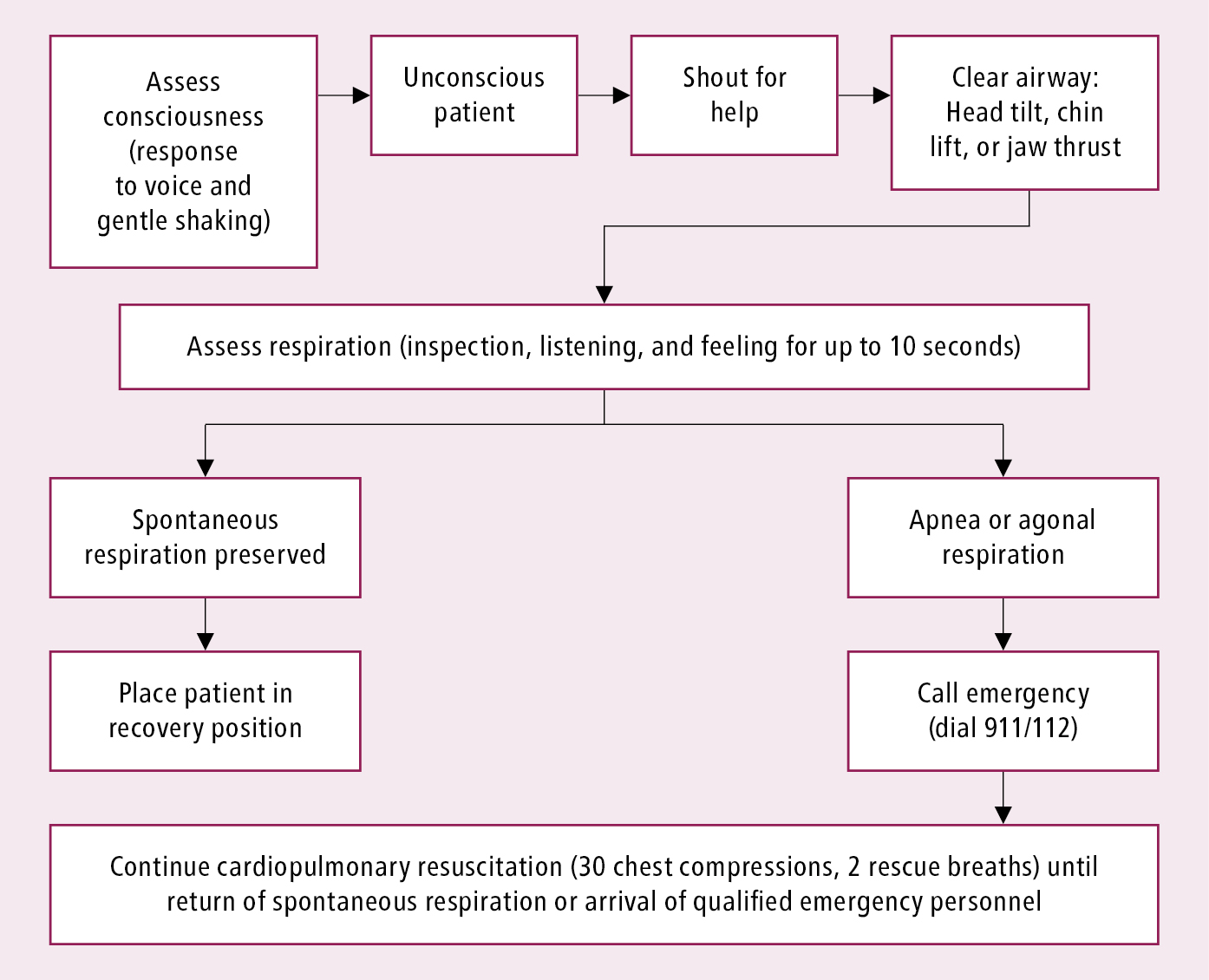
Figure 3.3-2. Basic life support algorithm. Adapted from Resuscitation. 2010;81(10):1219-76.
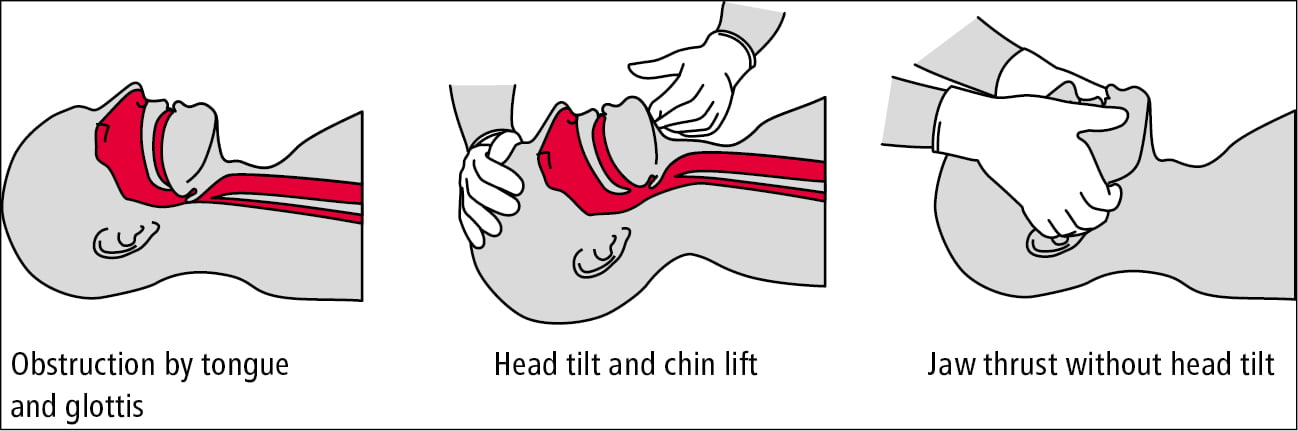
Figure 3.3-3. Clearing the airway.
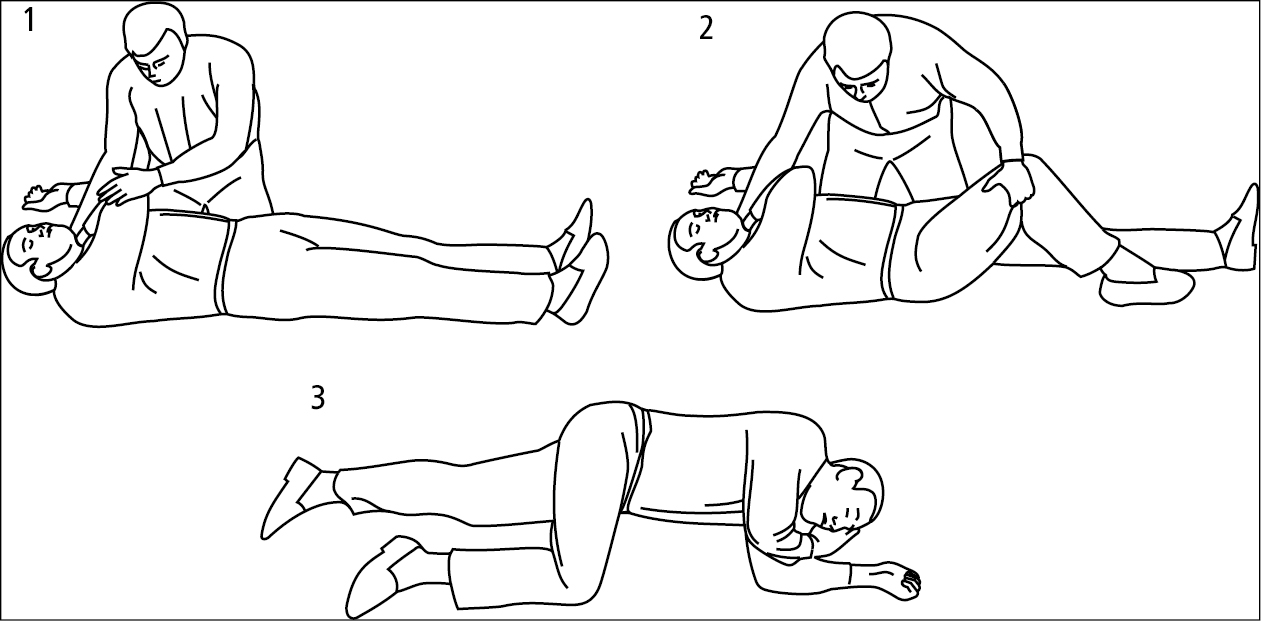
Figure 3.3-4. Placing an unconscious patient in the recovery position.
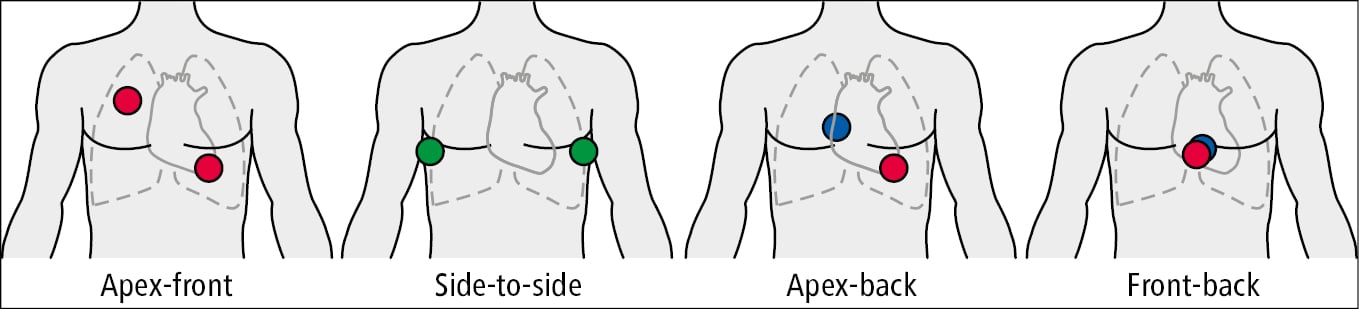
Figure 3.3-5. Recommended placement of electrodes for defibrillation. Location on the front (red), side (green), and back (blue) of the chest.
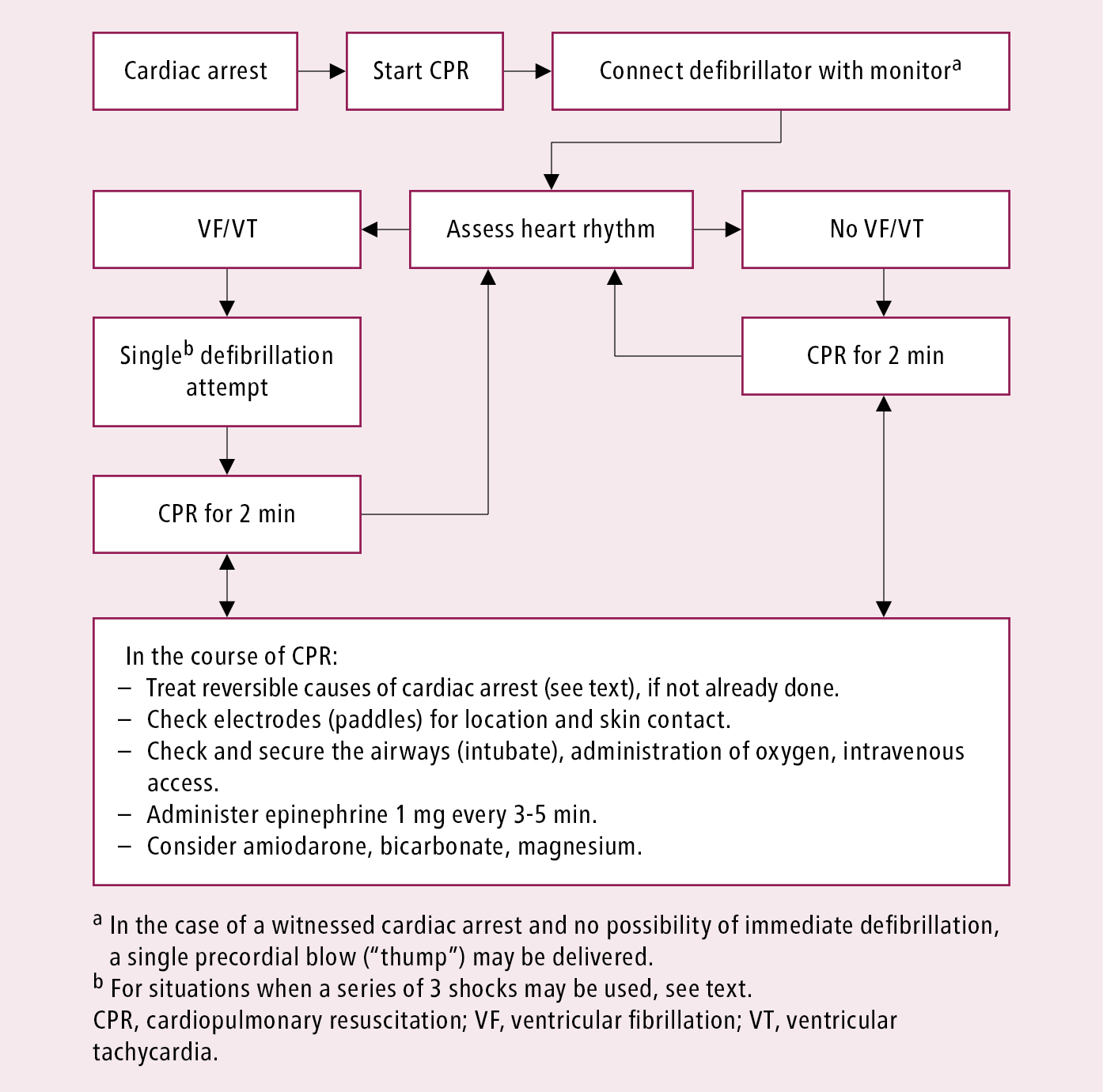
Figure 3.3-6. Advanced life support algorithm. Adapted from Resuscitation. 2010;81(10):1219-76.