Adler Y, Charron P, Imazio M, et al; European Society of Cardiology (ESC). 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC). Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015 Nov 7;36(42):2921-64. doi: 10.1093/eurheartj/ehv318. Epub 2015 Aug 29. PMID: 26320112.
Maron BJ, Udelson JE, Bonow RO, et al. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 3: Hypertrophic Cardiomyopathy, Arrhythmogenic Right Ventricular Cardiomyopathy and Other Cardiomyopathies, and Myocarditis: A Scientific Statement From the American Heart Association and American College of Cardiology. Circulation. 2015;132(22):e273-e280. doi:10.1161/CIR.0000000000000239. Epub 2015 Nov 2. PMID: 26621644.
Maisch B, Seferović PM, Ristić AD, et al; Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004 Apr;25(7):587-610. PMID: 15120056.
Definition, Etiology, PathogenesisTop
Pericardial syndromes refer to diseases that involve the pericardium. These include pericarditis, pericardial effusion, cardiac tamponade, pericardial masses, and constrictive pericarditis.
Pericarditis is the most common pericardial syndrome worldwide. It refers to an inflammatory process involving the pericardial sac.
Causes:
1) Infectious:
a) Viral: Parvovirus B19, Epstein-Barr virus, echovirus, coxsackievirus, cytomegalovirus, adenovirus, coronavirus disease 2019 (COVID-19).
b) Bacterial: Mycobacterium tuberculosis, Coxiella burnetii, Borrelia burgdorferi. Other bacterial causes are rare.
c) Fungal: Histoplasma spp, Aspergillus spp, Blastomyces spp, Candida spp. Fungal causes are rarely seen in immunocompetent patients.
2) Noninfectious:
a) Inflammatory: Post–myocardial infarction (MI) pericarditis (early after MI), postpericardiotomy syndrome after cardiac surgery.
b) Autoimmune diseases: Dressler syndrome (post–cardiac injury syndrome weeks after MI), systemic lupus erythematosus, rheumatoid arthritis, scleroderma, sarcoidosis, Sjögren syndrome, Behçet syndrome, other systemic vasculitides. Rarely pericarditis can be seen in familial Mediterranean fever and tumor necrosis factor (TNF) receptor-associated periodic syndrome.
c) Neoplastic: Primary tumors (rare; most frequently pericardial mesothelioma) or secondary tumors (common; most frequently lung cancer, breast cancer, lymphoma, melanoma).
d) Metabolic: Uremia, hypothyroidism (myxedema), anorexia nervosa, hypoadrenalism.
e) Traumatic and iatrogenic: Direct injury (penetrating thoracic injury, esophageal perforation); indirect injury (nonpenetrating thoracic injury, radiation injury); and other iatrogenic injury due to complications related to percutaneous coronary intervention (PCI), pacemaker lead insertion, or radiofrequency ablation.
f) Drug-related (rare): Procainamide, hydralazine, phenytoin, antineoplastic drugs (eg, doxorubicin, daunorubicin, cytarabine, fluorouracil, cyclophosphamide), penicillins, streptokinase, para-aminosalicylic acid, amiodarone, cyclosporine (INN ciclosporin), thiazide diuretics, granulocyte and macrophage colony-stimulating factors, TNF alpha inhibitors, and COVID-19 mRNA vaccines.
The mechanism for pericardial fluid accumulation in malignancy may be related to pericardial inflammation caused directly by cancer cells in the pericardium because of treatment (ie, certain chemotherapies or radiation) or obstruction of lymphatic drainage of pericardial fluid by malignant deposits.
Clinical Features and Natural HistoryTop
The natural history of acute pericarditis depends on etiology (Table 3.15-1). Pericarditis can be acute (<4-6 weeks), incessant (>4-6 weeks but <3 months with no remission), chronic (>3 months), or recurrent (recurring after an episode of acute pericarditis and following an asymptomatic period lasting ≥4-6 weeks; recurrence usually takes place within 18-24 months).
Adverse prognostic factors:
1) Major: Fever >38 degrees Celsius, subacute onset, large pericardial effusion, cardiac tamponade, lack of response to high-dose acetylsalicylic acid (ASA) or nonsteroidal anti-inflammatory drugs (NSAIDs) for ≥1 week.
2) Minor: Myopericarditis, immunosuppression, trauma, oral anticoagulant therapy.
Patients with ≥1 of the above adverse prognostic factors, either major or minor, are considered to be at high risk of complications. Patients at moderate risk have no risk factors but their response to NSAIDs is incomplete. Patients at low risk have no risk factors and good response to anti-inflammatory treatment.
1. Symptoms: In acute pericarditis symptoms include pleuritic and positional chest pain that is worse with inspiration and recumbency (the key symptom; see Chest Pain). This may be accompanied by dry cough and dyspnea and preceded by low-grade or high-grade fever (usually <39 degrees Celsius), malaise, arthralgia, and myalgia. Chronic pericarditis is characterized by chest pain, palpitations, loss of appetite, and sometimes weight loss.
2. Signs: Pericardial friction rub (transient, not always present; most easily audible during held expiration with the patient seated and leaning slightly forward). Cardiac tamponade may occur in patients with acute pericarditis (see Cardiac Tamponade). Features of myocarditis may be present in patients with infectious causes of pericarditis (see Myocarditis).
DiagnosisTop
1. Laboratory tests: Elevations in erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels, less frequently leukocytosis (in bacterial pericarditis), and sometimes elevated levels of cardiac troponins if associated with myocarditis (perimyocarditis).
2. Electrocardiography (ECG) (Figure 3.15-1): Generalized/diffuse upsloping ST-segment elevations and PR-segment depressions (except for lead aVR, where ST-segment depression and PR-segment elevation are seen in acute pericarditis). The evolution of pericarditis on ECG follows 4 stages: diffuse ST-elevation (stage 1); normalization of the ST segment over a few days (stage 2); T-wave inversions (stage 3); return to normal baseline ECG (stage 4). No pathologic Q-wave formation or precordial lead R-wave disappearance is observed (Figure 3.15-2).
3. Chest radiography (Figure 3.15-3): In patients with pericardial effusions >250 mL, the cardiac silhouette may be enlarged (the “water bottle” configuration if effusion is very large [see Figure 3.5-1]).
4. Echocardiography: Images may be normal. Pericardial effusion may be present. Transthoracic echocardiography (TTE) is recommended in all patients with suspected acute pericarditis to assess for the presence of pericardial effusion (end-diastolic echo-free space <10 mm [mild], 10-20 mm [moderate], >20 mm [severe], corresponding to ~50-100 mL, 100-500 mL, and >500 mL of fluid, respectively) and echocardiographic features of increased intrapericardial pressures or overt pericardial tamponade.
5. Computed tomography (CT): CT may be useful to detect pericardial calcification or thickening. Nongated CT scans generally overestimate the size of pericardial effusion (it is normally measured at end diastole but nongated CT obtains pictures throughout the cardiac cycle).
6. Analysis of pericardial fluid: Evaluation of pericardial fluid requires pericardiocentesis (see Pericardiocentesis).
7. Pericardial biopsy: Histologic examination of biopsy specimens is helpful in the diagnosis of pericarditis caused by neoplastic or inflammatory processes.
Diagnosis is based on clinical features and results of diagnostic tests, particularly echocardiography.
Acute pericarditis is diagnosed in patients fulfilling ≥2 out of 4 criteria:
1) Chest pain with features typical of pericarditis (ie, pleuritic, worse when lying flat).
2) Pericardial friction rub on auscultation.
3) New-onset widespread/diffuse ST-segment elevation and/or PR-segment depression on ECG (except for lead aVR, which is opposite, ie, ST depression and PR elevation).
4) Pericardial effusion on echocardiography (new-onset or worsening).
Further supportive findings of acute pericarditis include elevation of inflammatory markers (ESR or CRP) or imaging features suggestive of pericardial inflammation shown on CT or magnetic resonance imaging (MRI).
To confirm viral etiology (rarely needed), consider studies (histologic, cytologic, immunohistologic, molecular) of pericardial fluid and pericardial/epicardial biopsy. If diagnosis is uncertain, use the term “presumed viral pericarditis.” Routine viral serologic studies are not recommended except if HIV or hepatitis C virus is suspected to be the cause.
Malignancy can be confirmed as the cause of pericarditis or pericardial effusion based on pericardial fluid cytology, histology, and elevated tumor markers. High concentrations of carcinoembryonic antigen (CEA) with low adenosine deaminase (ADA) levels are typical for malignant effusions compared with those caused by tuberculosis (TB). These tests can also identify the primary tumor in the case of metastatic disease.
TreatmentTop
1. Patients at high or moderate risk of complications (see Clinical Features and Natural History, above) may be hospitalized to establish the etiology and monitor the course of disease. Low-risk patients may be treated on an outpatient basis with evaluation of response to anti-inflammatory treatment after ~1 week.
2. Management algorithm: Figure 3.15-4.
1. First-line agents in acute pericarditis:
1) ASA or NSAIDs with concomitant gastric protection (proton pump inhibitors). Dosage: Table 3.15-2.
2) Oral colchicine 0.5 to 0.6 mg (European tablets are 0.5 mg, North American tablets are 0.6 mg) bid for 3 months, usually in combination with a shorter course of ASA or NSAID. The dose may be given once daily in patients weighing <70 kg or those with gastrointestinal intolerance. Compared with placebo, colchicine reduces the risk of recurrence, improves remission rates, and decreases hospitalization rates.Evidence 1Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to the risk of bias. Imazio M, Gaita F, LeWinter M. Evaluation and Treatment of Pericarditis: A Systematic Review. JAMA. 2015 Oct 13;314(14):1498-506. doi: 10.1001/jama.2015.12763. Review. Erratum in: JAMA. 2015 Nov 10;314(18):1978. JAMA. 2016 Jan 5;315(1):90. Dosage error in article text. PubMed PMID: 26461998.
2. Glucocorticoids: To minimize adverse effects, low doses are used. Dosage: Table 3.15-2. Glucocorticoids are indicated when treatment with ASA or NSAIDs is contraindicated or ineffective and in situations where infection has been excluded or is unlikely. They are also used in patients who have specific indications for glucocorticoid treatment (eg, those with autoimmune disease, some patients with postpericardiotomy syndrome, and pregnant women). If infection cannot be excluded, particularly of bacterial etiology (including TB), do not use glucocorticoids. Colchicine is usually added to glucocorticoids.
3. Restriction of strenuous physical activity: In patients with acute pericarditis, strenuous physical activity should be restricted until symptoms, ECG findings, and elevated inflammatory markers (ESR or CRP) resolve. If there is evidence of concomitant myocarditis, strenuous activity should be avoided for ≥3 months, based on expert recommendations.
Treatment of Specific Types of Pericarditis
1. Purulent pericarditis: Open pericardial drainage through the substernal pericardiotomy approach with 0.9% saline irrigation and appropriate IV antimicrobial treatment. Consider intrapericardial administration of fibrinolytic agents and pericardiectomy in patients with significant adhesions, loculated or thick purulent effusion, recurrent cardiac tamponade, persistent infection, or disease progressing to constrictive pericarditis. This requires expert consultation and is performed by experienced operators.
2. Tuberculous pericarditis: Administration of 4 anti-TB drugs is necessary (see Tuberculosis: Active Disease). In patients not residing in endemic areas, empiric anti-TB treatment is not recommended if the diagnosis of TB pericarditis has not been confirmed. Empiric anti-TB treatment is recommended in residents of endemic areas with confirmed exudative pericardial effusion once other causes have been excluded. Some authors recommend addition of glucocorticoids: prednisone 1 to 2 mg/kg/d for 5 to 7 days with the dose gradually tapered down to discontinuation over 6 to 8 weeks.
3. Uremic pericarditis: Increasing the frequency of dialysis usually leads to the resolution of symptoms within 1 to 2 weeks. In patients with persistent symptoms use NSAIDs (with caution in patients with severe renal injury) and glucocorticoids. In patients with large pericardial effusions not responding to adequate treatment use intrapericardial glucocorticoids. Colchicine is contraindicated in patients with severe renal failure.
4. Pericarditis in patients with systemic connective tissue disease or sarcoidosis resolves with adequate treatment of the underlying condition. Intrapericardial glucocorticoids are not routinely recommended but may be considered in selected cases.
5. Post-MI pericarditis: ASA 650 mg every 4 hours for 2 to 5 days or ibuprofen (dosage: Table 3.15-2). Usually ASA is preferred, as these patients require antiplatelet therapy following MI.
6. Postpericardiotomy syndrome: NSAIDs or ASA in the same doses as in presumed viral pericarditis with colchicine for several weeks or months (even after the resolution of pericardial effusion). If ineffective, perform pericardiocentesis combined with intrapericardial administration of glucocorticoids and oral glucocorticoids for 3 to 6 months.
7. Neoplastic pericarditis: In patients with chemosensitive cancer use systemic chemotherapy. In patients with large effusions who are symptomatic, pericardiocentesis may be necessary. In patients with recurrent effusions consider administering an intrapericardial sclerosing agent (eg, tetracycline, bleomycin) or a nonsclerosing cytotoxic agent (eg, cisplatin; this is particularly effective in pericarditis caused by non–small cell lung cancer). Pericardial irradiation controls neoplastic effusions in >90% of cases of radiation-sensitive cancers (eg, lymphoma, leukemia) but it may by itself cause myocarditis or pericarditis (or both). Palliative treatment options include pericardiotomy or creation of a pericardial window.
8. Radiation pericarditis: Glucocorticoids. Dosage: Table 3.15-2.
9. Pericarditis in patients with hypothyroidism: Treatment of the underlying condition.
10. Recurrent pericarditis: First-line agents are (1) ASA or NSAID until complete symptom resolution and (2) colchicine for 6 months in combination. Alternatively, low-dose glucocorticoids may be used as in acute pericarditis (see above). Dosage: Table 3.15-2. The use of glucocorticoids is only recommended in patients who are refractory to ASA/NSAIDs and colchicine therapy. Sometimes colchicine treatment should be prolonged, depending on clinical response. Regularly perform follow-up measurements of serum CRP levels to establish the duration of therapy and response to treatment. When CRP levels normalize, gradually taper down the dose of anti-inflammatory medications while monitoring symptoms and CRP levels. Do not discontinue all agents at the same time. If symptoms of pericarditis recur in the period of tapering treatment, do not increase the dose of glucocorticoids and use maximal doses of ASA/NSAID instead (usually in divided doses every 8 hours) in addition to colchicine. Use analgesics for pain control. In glucocorticoid-dependent recurrent pericarditis in patients not responding to colchicine, consider IV immunoglobulins, anakinra, or azathioprine (this requires specialist consultation).
Follow-UpTop
In patients with recurrent or chronic pericarditis and in patients after surgical procedures on the pericardium, echocardiographic monitoring is indicated for early detection of cardiac tamponade or constrictive pericarditis.
ComplicationsTop
2. Constrictive pericarditis: A rare but serious complication of chronic pericarditis (particularly frequent in patients with bacterial or TB pericarditis), which is characterized by loss of elasticity of the pericardium.
Symptoms: Progressive weakness, chest pain, palpitations; signs of chronic systemic venous congestion (jugular vein distension, absence of jugular vein collapse during inspiration [Kussmaul sign], ascites, hepatic enlargement and pulsation, peripheral edema); early diastolic heart sound (pericardial knock); hypotension with low pulse pressure.
Diagnosis: Diagnosis is based on imaging studies: chest radiography (revealing pericardial calcifications [Figure 3.15-5], atrial enlargement, pleural effusion), CT, MRI, and echocardiography. Intracardiac pressure measurements may also be performed. ECG may reveal low-amplitude QRS complexes, generalized T-wave inversions or T-wave flattening, widening of P waves, sometimes atrial fibrillation, atrioventricular conduction disturbances, or intraventricular conduction disturbances. However, ECG may also be normal.
Differential diagnosis: Restrictive cardiomyopathy. Differentiation is based on echocardiography (including tissue Doppler echocardiography), CT, MRI, and cardiac catheterization.
Treatment: Pericardiectomy.
Tables and FiguresTop
|
|
Viral |
Bacterial |
Tuberculous |
Autoimmune |
|
Spontaneous remission |
Frequent |
Never |
Never |
Rare |
|
Relapse rates |
30%-50% |
Rare |
Frequent |
Frequent (>25%) |
|
Mortality rates in untreated disease |
Depends on virus type and occurrence of cardiac tamponade |
100% |
85% |
Death in case of untreated cardiac tamponade |
|
Constriction |
Rare |
Frequent |
Frequent |
Rare |
|
Agent |
Dosage |
|
|
Acute pericarditis |
Recurrent pericarditis |
|
|
ASA |
650-1000 mg every 6-8 ha,b |
500-1000 mg every 6-8 h (1.5-4 g/d)b,c |
|
Ibuprofen |
600-800 mg every 8 ha,d |
600 mg every 8 h (1200-2400 mg)b,c |
|
Colchicine |
0.5-0.6 mg (once dailye or bidf)g,h |
0.5-0.6 mg (bidf or once dailye,i)h,j |
|
Indomethacin |
– |
25-50 mg every 8 hc,k,l |
|
Glucocorticoids |
Doses depend on agents usedm,n |
|
|
a For 1-2 weeks. b Decrease the dose by 250-500 mg every 1-2 weeks. In case of recurrent pericarditis in patients showing more resistance to treatment, you may consider more gradual and longer tapering of doses down to discontinuation. c For weeks or months. d Decrease the dose by 200-400 mg every 1-2 weeks. In case of recurrent pericarditis in patients showing more resistance to treatment, you may consider more gradual and longer tapering of doses down to discontinuation. e In patients <70 kg. f In patients ≥70 kg. g For 3 months. Note that in North America colchicine is only available in 0.6 mg tablets, whereas the 0.5 mg dose is available in Europe. h Tapering down is not necessary. However, you may decrease the dose by 0.5 mg every other day in patients <70 kg or by 0.5 mg once a day in the last weeks of treatment in patients ≥70 kg. i In patients who do not tolerate higher doses. j For ≥6 months. k Start from low doses and titrate them up to avoid headache and dizziness. l Decrease the dose by 25 mg every 1-2 weeks. In patients resistant to treatment, you may consider more gradual and longer tapering of doses down to discontinuation. m The starting dose of prednisone is 0.25-0.5 mg/kg/d. A dose of 25 mg of prednisone is equivalent to 20 mg of methylprednisolone. Higher doses should be avoided except for selected patients (higher doses are then used over a few days and rapidly tapered down to 25 mg/d). n Prednisone dose may be tapered down (particularly <25 mg/d) when symptoms have resolved and CRP has normalized. |
||
|
Based on Eur Heart J. 2015;36(42):2921-64. |
||
|
ASA, acetylsalicylic acid; bid, twice a day; CRP, C-reactive protein. |
||
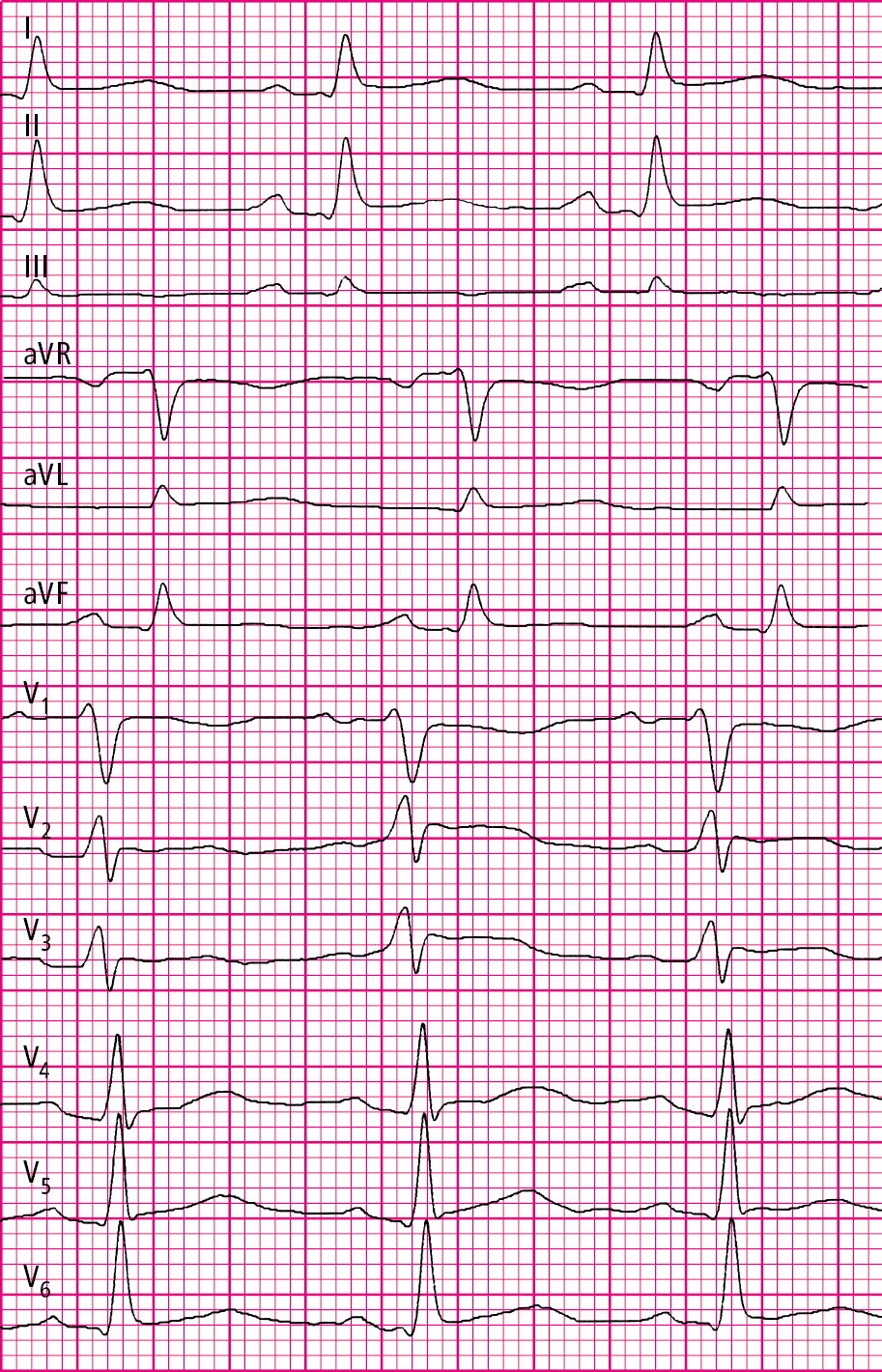
Figure 3.15-1. Echocardiography of a patient with acute pericarditis: PR-segment depressions and ST-segment elevations in all leads (paper speed, 50 mm/s).
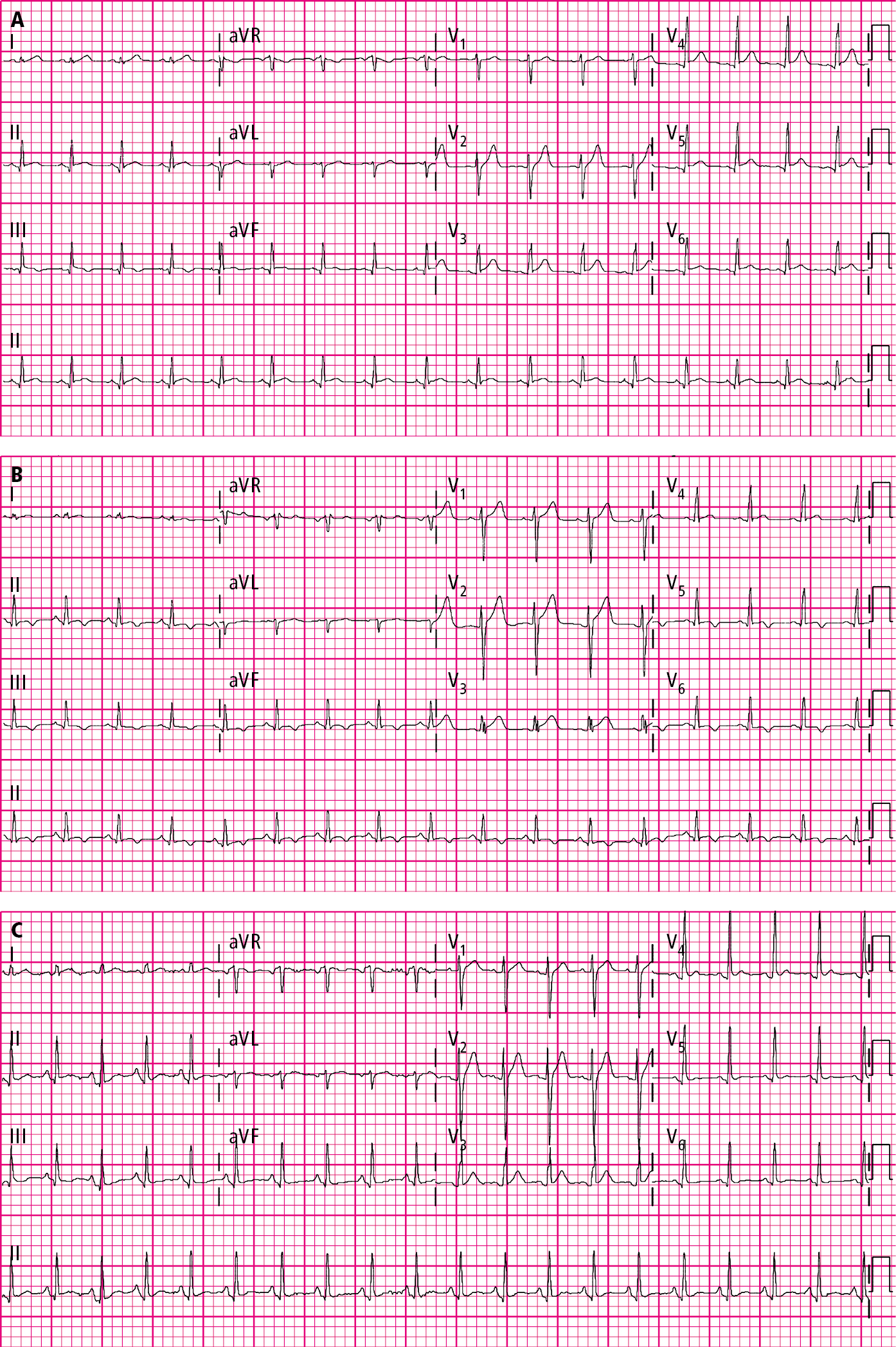
Figure 3.15-2. Classic electrocardiography (ECG) evolution in acute pericarditis. The initial ECG shows a diffuse ST-segment elevation and PR depression (A), which is followed by the resolution of the ST-segment elevation and then the presence of diffuse T-wave inversion (B), and lastly by improvement of all ECG changes (C). Figures courtesy of Dr Hassan Mir.
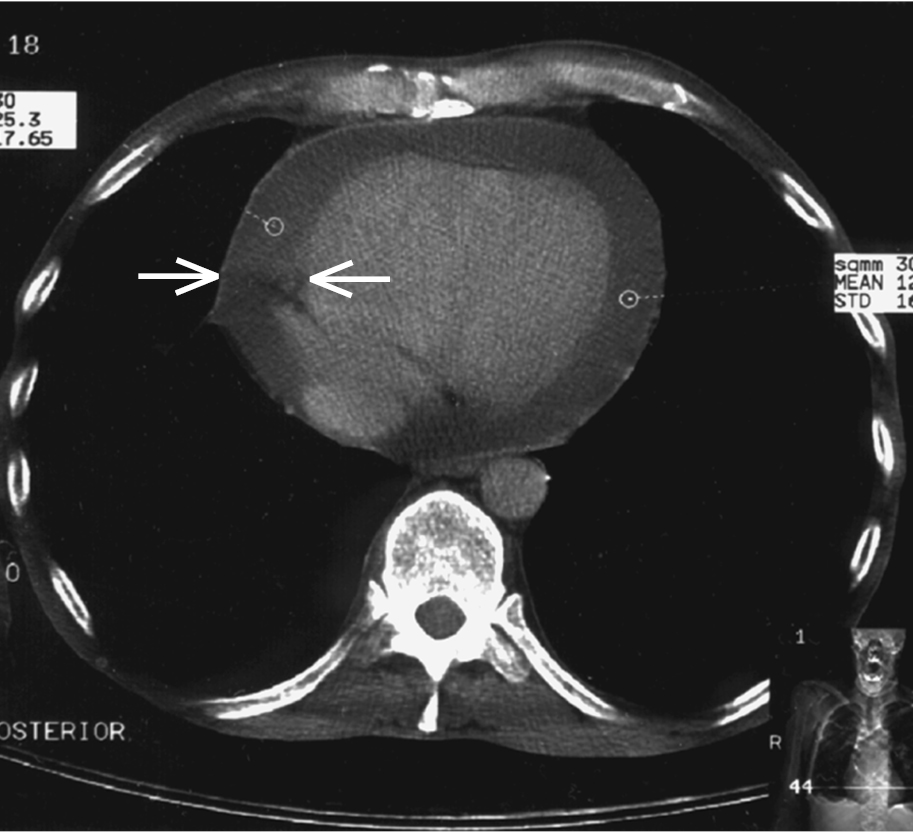
Figure 3.15-3. Chest computed tomography (CT): pericardial effusion (arrows) with a fluid layer up to 18 mm.
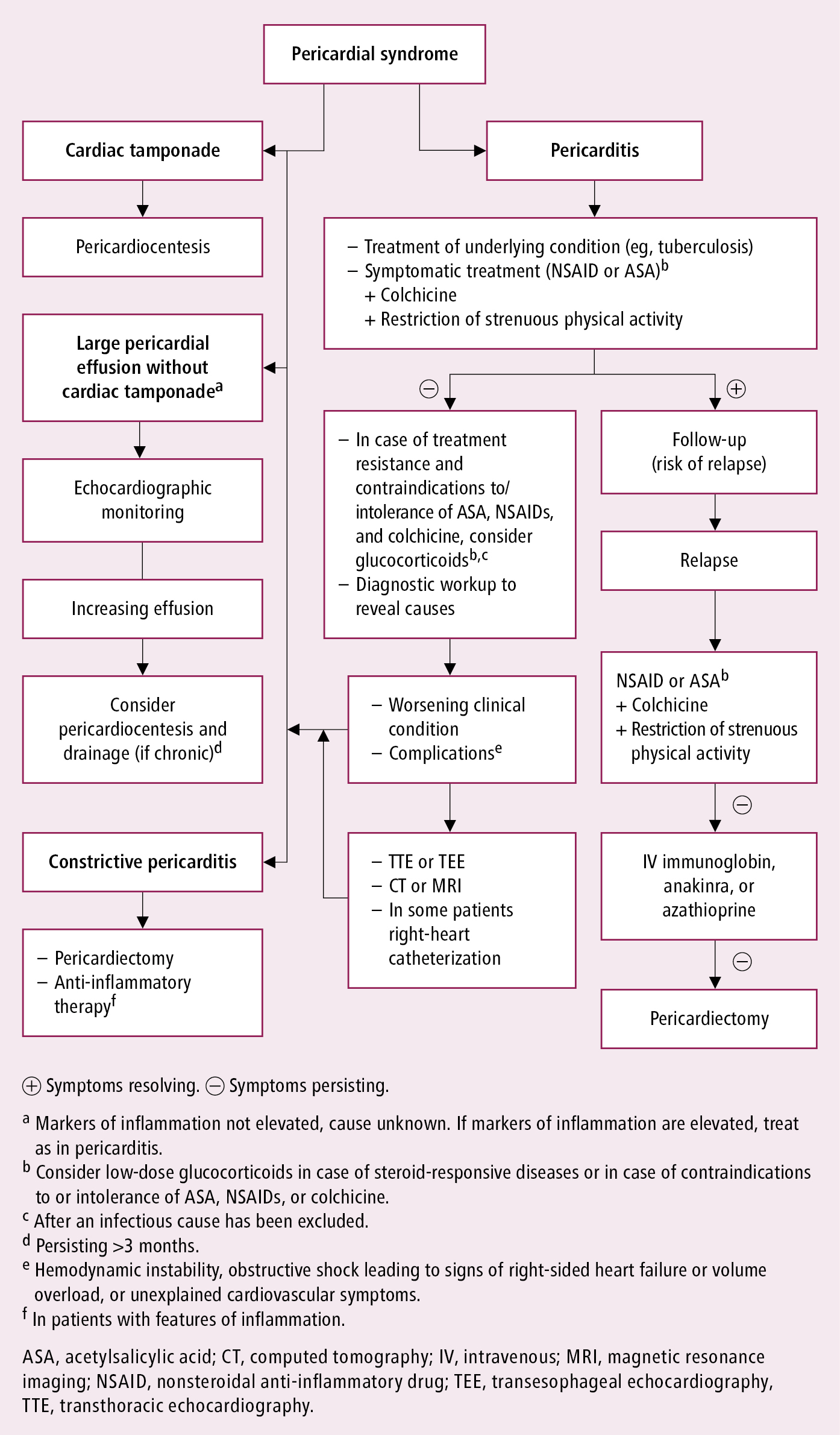
Figure 3.15-4. Management algorithm in pericarditis. Based on the 2015 European Society of Cardiology guidelines.
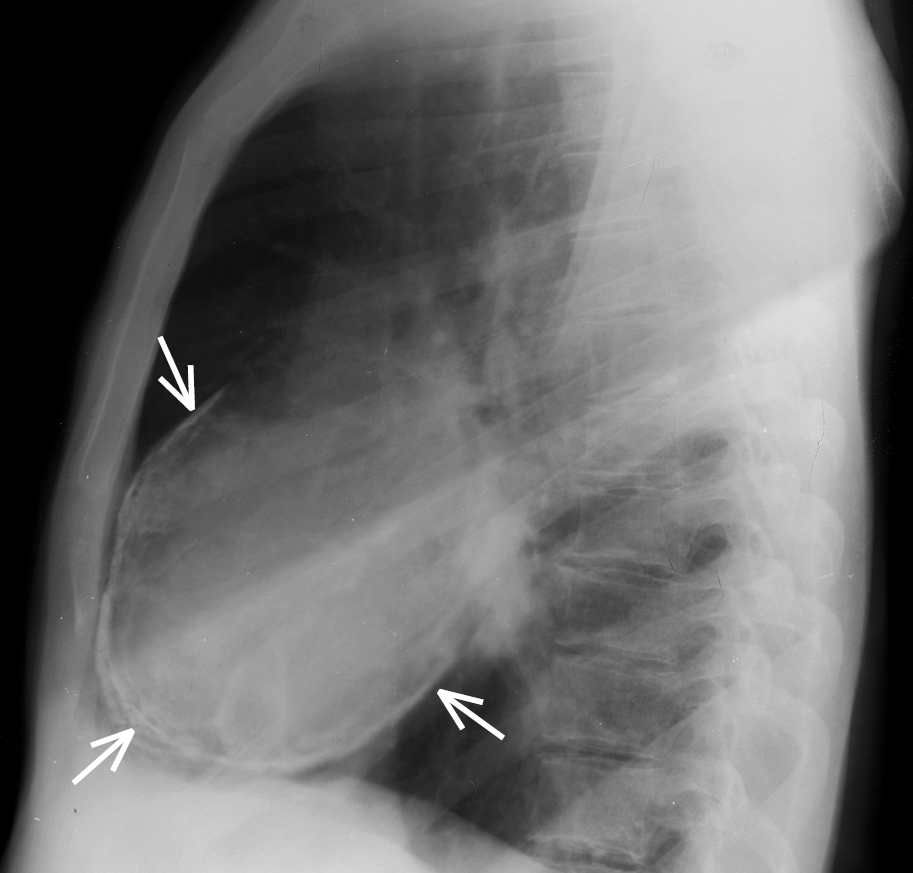
Figure 3.15-5. Chest radiography, lateral view: pericardial calcification (arrows).