Dr Roman Jaeschke asks Dr James Douketis, an expert in thromboembolism and anticoagulation, about takeaways from a recent publication on anticoagulation in patients with intracranial hemorrhage, focusing on questions regarding when and how to restart therapy.
References
Ivany E, Ritchie LA, Lip GYH, Lotto RR, Werring DJ, Lane DA. Effectiveness and Safety of Antithrombotic Medication in Patients With Atrial Fibrillation and Intracranial Hemorrhage: Systematic Review and Meta-Analysis. Stroke. 2022 Oct;53(10):3035-3046. doi: 10.1161/STROKEAHA.122.038752. Epub 2022 Jul 8. PMID: 35862238.For a Publications of the Week article discussing the paper, click here.
Roman Jaeschke, MD, MSc: Good morning, welcome to another edition of McMaster Perspective. We are meeting with my friend and colleague Dr Jim Douketis, a specialist and leader in thromboembolism and also in the risks of anticoagulation in different areas of medicine.
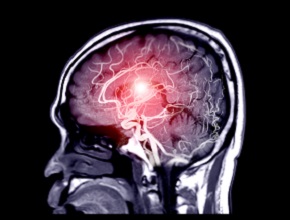
Today’s recording is made on the basis of a systematic review and meta-analysis dealing with a problem that is reasonably frequent, which is a person who is on anticoagulation for good reasons and is suffering a nontraumatic intracranial hemorrhage. And immediately the question comes: should we restart, when should we restart, and how should we conduct the anticoagulation down the road. Dr Douketis?
James Douketis, MD: Thank you very much for bringing this topic up, Roman. It does come up relatively frequently and it’s a very challenging area. I think the meta-analysis that we’re discussing today provides one piece of that puzzle in terms of decision making. If you look at it just on face value, I think the message of the meta-analysis is that your default management should be to restart anticoagulation in patients who have an indication for anticoagulation and yet they have suffered an intracranial hemorrhage. But there are important things that the meta-analysis does not discuss. That’s important, I think, for clinical decision making.
Roman Jaeschke: So what would be the practical advice to clinicians? I do not think it would be “Don’t worry, restart it.” Could you expand on it?
James Douketis: I would be happy to because it is not a kind of black-and-white, one-size-fits-all approach. In general, as a clinician, what you want to do in anybody who has a serious life-threatening or, in this case, an intracranial hemorrhage is try to ascertain, the best you can, what the etiology is. The etiology will often drive the risk for recurrent bleeding and in turn will determine the safety and the timing of reanticoagulation. So that’s the first thing.
Once you’ve done that, you have to discuss—and I do this routinely—with a stroke neurologist or a neurosurgeon as to the timing of safe reanticoagulation.
Then the third step I look at is the type of anticoagulant. What was the patient taking before? Were they on a vitamin K antagonist like warfarin? Were they on a direct oral anticoagulant (DOAC)? And is there a safer option or a safer intensity of anticoagulation?
And the final thing I do, the fourth step, is not to forget: Are there other factors that we can consider to reduce the risk of intracranial hemorrhage, independent of anticoagulant management? And, of course, the one that comes to mind for all of us is good blood pressure control. We know that if we control blood pressure in general terms, this will reduce patients’ risk of intracranial hemorrhage.
Roman Jaeschke: Let me drill you a little bit more about details. The first thing is, from all we know, are there safer and less safe anticoagulants in this setting?
James Douketis: The general dichotomy in terms of safety separates vitamin K antagonists from DOACs. So in general I think if a patient was previously on a vitamin K antagonist, then it would make sense to switch them to a DOAC. Within that category, we don’t have enough studies to definitively say that one agent is better at preventing recurrent intracranial hemorrhage compared with another DOAC. But that would be my general advice, and the corollary to that is to make sure that they are receiving the correct dose. Often we see patients are not on the correct dose of a DOAC because clinicians fear having their patient have a bleed and often underdose at the expense of exposing them to an increased risk for stroke and other thromboembolic events.
Roman Jaeschke: So the first answer is which one to use. The second one: how do you judge the risk of not anticoagulating? Is there any fast practical advice you could give?
James Douketis: In any area of anticoagulant management, we’re always balancing risk for stroke or thromboembolism against risk for bleeding or, in this case, recurrent bleeding. To borrow a tennis analogy, we want to try to find that sweet spot where the risk for stroke is being diminished, as is the risk for bleeding. Of course, every patient is different and that’s why I think this meta-analysis helps, but in a way it’s a very crude analysis. This area requires very specific, individualized management.
Let me give you an example. If we had a patient who had a mechanical heart valve and suffered an intracranial bleed, and we ascertained that this was due to a fall and led to a subdural hematoma requiring surgical evacuation, that person would be much more prone to recurrent thromboembolism than recurrent bleeding, so we would be likely to reanticoagulate them quicker. Under those circumstances, we’ve got a transient, reversible type of bleeding. And we have a patient, let’s say, with a mechanical mitral valve at high risk for thromboembolism.
Let me give you a different example. A patient with atrial fibrillation now comes in with an intracerebral hemorrhage, so within the cortex. And we ascertain based on magnetic resonance imaging (MRI) studies that they probably have amyloid angiopathy—an infrequent but very serious vasculopathy that is associated with a high risk for rebleeding. And in that individual we may say any form of anticoagulation is not safe and maybe we need to resort to an antiplatelet agent. So, very individualized management. I can’t stress enough the importance of looking at each patient separately and discussing them with one or more neurological specialists.
Roman Jaeschke: The practical message, if I got one, is your default should be to try to restart, taking into account the safety measures, which you mentioned, and, if you have access to, consulting with both a neurologist or stroke neurologist and potentially a neurosurgeon; obviously not everybody has access to it.
The other thing that you mentioned is the risk of stroke due to an underlying condition. Even atrial fibrillation in one person carries a different risk than in another person, depending on the usual CHA2DS2-VASc score criteria.
So [there are] the risks of recurrent stroke, the risks of bleeding, the accessibility to some more specialized advice, and the choice of an anticoagulant. But still, the issue is to try to restart if possible, correct?
James Douketis: Yes, that is the one overarching takeaway message. It is anchored not just on studies that have looked at intracranial bleeding but also gastrointestinal (GI) bleeding and bleeding elsewhere in patients who were previously anticoagulated. Although all of these studies were observational, so they looked at patients who were restarted or not restarted on anticoagulants in a nonrandomized manner, the totality of evidence in all of these patient populations—whether GI or intracranial bleeding—is very similar. The benefits of restarting in terms of reducing stroke and thromboembolism and, importantly, reducing overall mortality outweigh the risks of recurrent bleeding. But as we’ve discussed, there are a few caveats with that and this is definitely not a one-size-fits-all approach.
Roman Jaeschke: Thank you very much. We invite our users and readers to look at the Publications of the Week article on the same subject and access the original article if they wish. Thank you very much, Dr Douketis, I appreciate this.
James Douketis: It’s my pleasure.
 English
English
 Español
Español
 українська
українська