The best method of thromboprophylaxis in patients with fractures
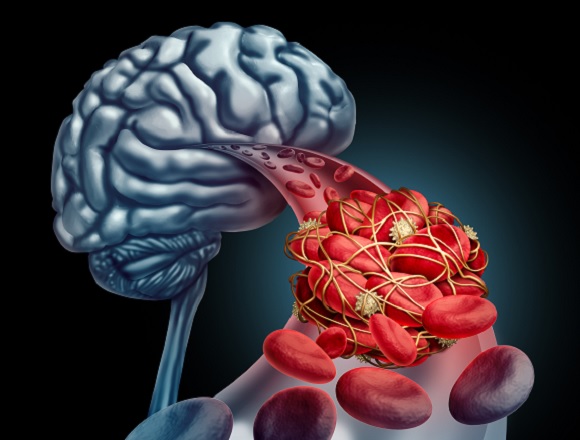
Background: There is uncertainty about the best method of thromboprophylaxis in patients with fractures.
Methods: This was a randomized noninferiority trial that enrolled adults (age ≥18 years) who sustained a surgically treated fracture that involved the hip to midfoot or shoulder to wrist, or any fracture of the pelvis or acetabulum. Patients were randomly allocated, in an open-label manner, to receive thromboprophylaxis with low-molecular-weight heparin (LMWH; enoxaparin) 30 mg bid or acetylsalicylic acid (ASA) 81 mg bid during hospitalization.
Post discharge, patients continued the allocated thromboprophylaxis but with a duration based on local practices. The primary study outcome was death from any cause at 90 days. Secondary outcomes were deep vein thrombosis (DVT), nonfatal pulmonary embolism (PE), and bleeding.
Results: In total, 12,211 patients were studied (mean age, 44.6 years; 62.3% men), some of whom had prior venous thromboembolism (<1%) and cancer (2.5%). Patients received a mean (±SD) of 8.8±10.6 in-hospital thromboprophylaxis doses and were prescribed a median 21-day supply of thromboprophylaxis at discharge. Death occurred in 0.73% of patients in the LMWH group and in 0.78% of patients in the ASA group (difference, 0.05%; 96.2% CI, -0.27 to 0.38; P < .001 for a noninferiority margin of 0.75%). DVT occurred in 1.71% of patients in the LMWH group and in 2.51% in the ASA group (difference, 0.80%; 95% CI, 0.28-1.31). PE occurred in 1.49% of patients in each group; bleeding complications (~14%) and other serious adverse events were similar in the two groups.
Conclusions: The authors concluded that in patients with surgically treated extremity fractures or with any pelvic or acetabular fracture thromboprophylaxis with ASA was noninferior to LMWH in preventing death and was associated with low rates of DVT and PE.
McMaster editors’ commentary: Decades ago, ASA was studied as a thromboprophylaxis agent after orthopedic surgery, but it was deemed inferior to LMWH, whereas it is currently widely used (following 5 days of an anticoagulant) after hip and knee replacement surgery and as a standalone agent in patients with below-knee fractures.
What has changed? Most importantly, patients are ambulatory far earlier after orthopedic surgery, typically starting on the day of surgery. Other factors include better surgical and anesthetic techniques. This has allowed an antiplatelet agent (ASA) to have comparable efficacy as anticoagulant options.
In the METRC study, ASA appears to have gained another “therapeutic win,” but there are caveats. First, as the population studied was young (mean age, 44 years), with low rates of comorbidities associated with thrombosis risk, the results may not be applicable to older patients, especially those aged ≥70, 80, or 90 years with traumatic (falls-related) hip and pelvic fractures. Second, data were not separated according to fracture type and caution should be considered when applying the results to fractures associated with a high thrombosis risk (hip, pelvis).
On balance, ASA is gaining traction as a standalone thromboprophylaxis method, which is a “win” for patients due to its wide availability and low cost.
 English
English
 Español
Español
 українська
українська