Effectiveness and safety of antithrombotic medication in patients with atrial fibrillation and intracranial hemorrhage
For a McMaster Perspective interview discussing this topic, click here.
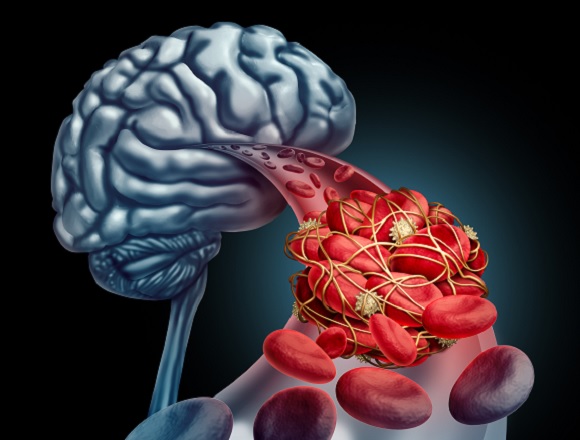
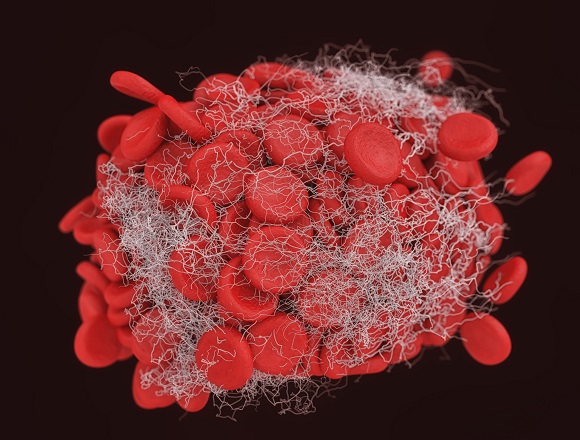
Background: The management of patients with atrial fibrillation (AF) who develop an intracranial hemorrhage (ICH) is challenging in terms of whether to withhold or, alternatively, resume or initiate anticoagulant therapy. This decision is anchored on an assessment of patients’ risk of stroke and other thromboembolic events as well as recurrent ICH.
Methods: This systematic review assessed the effectiveness and safety of using anticoagulants after a nontraumatic ICH in patients with AF. Twenty studies, totaling 50,470 patients, were included, of which only 2 were randomized controlled trials (totaling 304 patients), with the remainder being observational studies.
Results: After ICH, the use of anticoagulant therapy was associated with a significant reduction in thromboembolic events (relative risk [RR], 0.51; 95% CI, 0.30-0.86) and all-cause mortality (RR, 0.52; 95% CI, 0.38-0.71) and was not associated with a significant increased risk of recurrent ICH (RR, 1.44; 95% CI, 0.38-5.46) compared with no therapy. Compared with warfarin therapy, the use of a direct oral anticoagulant (DOAC) was more effective at reducing the risk of thromboembolic events (RR, 0.65; 95% CI, 0.44-0.97) and conferred a lower risk of recurrent ICH (RR, 0.52; 95% CI, 0.40-0.67).
Conclusions: The authors concluded that in patients after nontraumatic nonfatal ICH who have AF initiating anticoagulant therapy is associated with a reduced risk of thromboembolism and mortality without significantly increasing the risk of recurrent ICH.
McMaster editors’ commentary: This study supports the widely held premise that patients who have had an ICH and have an ongoing or new clinical indication for anticoagulant therapy, most commonly AF, should be considered for initiation or resumption of anticoagulation. What this study does not address is when it is safe to initiate or resume anticoagulant therapy, although it does suggest to use a DOAC over warfarin. This decision is highly individualized, based on incorporating a patient’s risk of stroke or another thromboembolic event if anticoagulation is withheld coupled with the risk of recurrent ICH if anticoagulant therapy is administered. Moreover, there are some patients in whom the use of anticoagulant therapy is prohibitive (eg, if the ICH is associated with amyloid angiopathy or malignant disease). The location of the ICH will determine when anticoagulant therapy can be initiated. In general, this occurs 2 to 6 weeks after bleeding: earlier after subdural, later after subcortical (basal ganglia, corona radiata), and latest after cortical (hemispheric) hemorrhage; the size of the ICH also affects the timing of anticoagulant therapy initiation. Given the complexity of factors involved in this clinical decision, consultation with various specialists, especially neurologists, neurosurgeons, or both, is advisable.
 English
English
 Español
Español
 українська
українська