References
Fischer U, Koga M, Strbian D, et al; ELAN Investigators. Early versus Later Anticoagulation for Stroke with Atrial Fibrillation. N Engl J Med. 2023 Jun 29;388(26):2411-2421. doi: 10.1056/NEJMoa2303048. Epub 2023 May 24. PMID: 37222476.For a McMaster Perspective interview with Dr Aristeidis Katsanos on the use of DOACs in patients with AF after ischemic stroke, click here.
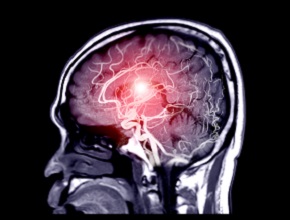
Background: In patients with atrial fibrillation (AF) who develop an ischemic stroke, the risks and benefits of early versus later initiation of direct oral anticoagulants (DOACs) are uncertain. Earlier initiation of anticoagulant therapy may reduce the risk of stroke progression or recurrence but may also increase the risk of hemorrhagic transformation of the stroke.
Methods: This was an open-label, multicenter randomized trial in patients with AF and ischemic stroke. The patients were allocated to early anticoagulation initiation, defined as anticoagulation within 48 hours after a minor or moderate-severity stroke or 6 to 7 days after a major stroke; or later anticoagulation initiation, defined as 3 to 4 days after a minor stroke, 6 to 7 days after a moderate stroke, or 12 to 14 days after a major stroke. The primary study outcome was a composite of recurrent ischemic stroke, systemic embolism, major extracranial bleeding, symptomatic intracranial hemorrhage, or vascular death within 30 days after randomization. Secondary outcomes included the components of the composite primary outcome at 30 and 90 days.
Results: There were 2013 patients studied, of whom 37% had a minor stroke, 40% had a moderate-severity stroke, and 23% had a major stroke. The primary study outcome occurred in 2.9% (n = 29) of patients in the early-anticoagulation group and in 4.1% (n = 41) of patients in the later-anticoagulation group (risk difference, -1.18% percentage points; 95% CI, -2.84 to 0.47). Recurrent ischemic stroke occurred in 1.4% (n = 14) of patients in the early-anticoagulation group and in 2.5% (n = 25) of patients in the later-anticoagulation group (odds ratio [OR], 0.57; 95% CI, 0.29-1.07) by 30 days, and in 1.9% (n = 18) and 3.1% (n = 30) of patients, respectively, by 90 days (OR, 0.60; 95% CI, 0.33-1.06). Symptomatic intracranial hemorrhage occurred in 0.2% (n = 2) patients in both groups.
Conclusions: The authors concluded that the incidence of recurrent ischemic stroke, systemic embolism, major extracranial bleeding, symptomatic intracranial hemorrhage, or vascular death at 30 days was estimated at 2.8 percentage points lower to 0.5 percentage points higher with early initiation of DOAC therapy as compared with the later start.
McMaster editors’ commentary: In patients with ischemic stroke occurring in association with AF, the “1-3-6-12-day rule” can be used to guide when to initiate anticoagulation and corresponds to stroke severity classified as transient ischemic attack (TIA), minor, moderate, and severe. The present study used an adaptation of this rule and was based on brain imaging (not neurologic deficit) to define stroke severity. Importantly, patients with a TIA were excluded. This study supports the safety of earlier anticoagulant initiation with DOACs in patients with minor to moderate (<48 h) and major (6-7 days) stroke.
This finding is clinically important because DOACs have a rapid onset of action but, unlike heparins or vitamin K antagonists, narrower single-clotting factor (IIa or Xa) inhibition, which may explain the lower risk of intracranial hemorrhage and, in the case of acute ischemic stroke, potentially lower rates of hemorrhagic transformation.
 English
English
 Español
Español
 українська
українська